UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
WASHINGTON, D.C. 20549
FORM 8-K
CURRENT REPORT
Pursuant to Section 13 or 15(d)
of the Securities Exchange Act of 1934
Date of Report (Date of earliest event reported): October 17, 2024
Aura Biosciences, Inc.
(Exact name of Registrant as Specified in Its Charter)
| Delaware | 001-40971 | 32-0271970 | ||
| (State or Other Jurisdiction of Incorporation) |
(Commission File Number) |
(IRS Employer Identification No.) |
||
| 80 Guest Street | ||||
| Boston, Massachusetts | 02135 | |||
| (Address of Principal Executive Offices) | (Zip Code) | |||
Registrant’s Telephone Number, Including Area Code: 617 500-8864
Not Applicable
(Former Name or Former Address, if Changed Since Last Report)
Check the appropriate box below if the Form 8-K filing is intended to simultaneously satisfy the filing obligation of the registrant under any of the following provisions:
| ☐ | Written communications pursuant to Rule 425 under the Securities Act (17 CFR 230.425) |
| ☐ | Soliciting material pursuant to Rule 14a-12 under the Exchange Act (17 CFR 240.14a-12) |
| ☐ | Pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act (17 CFR 240.14d-2(b)) |
| ☐ | Pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act (17 CFR 240.13e-4(c)) |
Securities registered pursuant to Section 12(b) of the Act:
| Title of each class |
Trading Symbol(s) |
Name of each exchange on which registered |
||
| Common Stock, $0.00001 par value per share | AURA | The Nasdaq Global Market |
Indicate by check mark whether the registrant is an emerging growth company as defined in Rule 405 of the Securities Act of 1933 (§ 230.405 of this chapter) or Rule 12b-2 of the Securities Exchange Act of 1934 (§ 240.12b-2 of this chapter).
Emerging growth company ☒
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ☐
| Item 7.01. | Regulation FD Disclosure. |
On October 17, 2024, Aura Biosciences, Inc. (the “Company”) announced positive early data from its ongoing Phase 1 clinical trial of bel-sar (AU-011) in patients with non-muscle-invasive bladder cancer (“NMIBC”). The Company issued a press release announcing this update titled “Multiple Clinical Complete Responses Demonstrated Following Single Low Dose Administration of Bel-sar in Patients with Non-Muscle-Invasive Bladder Cancer (NMIBC) in Ongoing Phase 1 Trial”. A copy of the press release is furnished herewith as Exhibit 99.1 and is incorporated herein by reference.
The information furnished under this Item 7.01, including Exhibit 99.1 hereto, shall not be deemed “filed” for purposes of Section 18 of the Securities Exchange Act of 1934, as amended (the “Exchange Act”), or otherwise subject to the liabilities of that section, nor shall it be deemed incorporated by reference in any filing under the Securities Act of 1933, as amended, or the Exchange Act, except as expressly set forth by specific reference in such a filing.
| Item 8.01 | Other Events. |
On October 17, 2024, the Company hosted a virtual urologic oncology investor event to present early NMIBC data from its ongoing Phase 1 trial. A copy of the presentation from this event is filed as Exhibit 99.2 for purposes of Section 18 of the Exchange Act.
Forward Looking Statements
Statements contained under this Item 8.01 regarding matters that are not historical facts are “forward-looking statements” within the meaning of the Private Securities Litigation Reform Act of 1995. Because such statements are subject to risks and uncertainties, actual results may differ materially from those expressed or implied by such forward-looking statements. Such statements include, but are not limited to, statements about the initiation, timing, progress, results and cost of the Company’s research and development programs and the Company’s current and future preclinical studies and clinical trials, including statements regarding the timing of initiation and completion of studies or trials and related preparatory work, the period during which the results of the trials will become available and the Company’s research and development programs; statements regarding the Company’s expectations for an improved quality of life of patients after treatment with bel-sar and changes to the treatment paradigm for patients; statements regarding the Company’s beliefs and expectations for the high unmet medical need for an effective local treatment in urologic oncology to preserve organ function; and the size and growth potential of the markets for the Company’s product candidates and the Company’s ability to serve those markets.
Any forward-looking statements are neither promises nor guarantees, and investors should not place undue reliance on these forward-looking statements because they involve known and unknown risks, uncertainties, and other factors, many of which are beyond the Company’s control and which could cause actual results to differ materially from those expressed or implied by these forward-looking statements, including, without limitation, uncertainties inherent in clinical trials and in the availability and timing of data from ongoing clinical trials; the expected timing for submissions for regulatory approval or review by governmental authorities; the risk that the results of the Company’s preclinical and clinical trials may not be predictive of future results in connection with future clinical trials; the risk that interim or early data from ongoing clinical trials may not be predictive of final data from completed clinical trials; the risk that governmental authorities may disagree with the Company’s clinical trial designs even where the Company has obtained agreement with governmental authorities on the design of such trials; whether the Company will receive regulatory approvals to conduct trials or to market products; whether the Company’s cash resources will be sufficient to fund its foreseeable and unforeseeable operating expenses and capital expenditure requirements; the Company’s ongoing and planned preclinical activities; and the Company’s ability to initiate, enroll, conduct or complete ongoing and planned clinical trials. These risks, uncertainties, and other factors include those risks and uncertainties described under the heading “Risk Factors” in the Company’s most recent Annual Report on Form 10-K and Quarterly Report on Form 10-Q filed with the United States Securities and Exchange Commission (“SEC”) and in subsequent filings made by the Company with the SEC, which are available on the SEC’s website at www.sec.gov. Except as required by law, the Company disclaims any intention or responsibility for updating or revising any forward-looking statements contained under this Item 8.01 in the event of new information, future developments or otherwise. These forward-looking statements are based on the Company’s current expectations and speak only as of the date hereof and no representations or warranties (express or implied) are made about the accuracy of any such forward-looking statements.
| Item 9.01 | Financial Statements and Exhibits. |
(d) Exhibits.
| Exhibit |
Description |
|
| 99.1 | Press Release Dated October 17, 2024. | |
| 99.2 | Virtual Urologic Oncology Investor Event Presentation of the Company. | |
| 104 | Cover Page Interactive Data File (embedded within the Inline XBRL document). | |
SIGNATURES
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned hereunto duly authorized.
| Aura Biosciences, Inc. | ||||||
| Date: October 17, 2024 | By: | /s/ Elisabet de los Pinos |
||||
| Elisabet de los Pinos | ||||||
| President and Chief Executive Officer | ||||||
Exhibit 99.1
Multiple Clinical Complete Responses Demonstrated Following Single Low Dose Administration of Bel-sar in Patients with Non-Muscle-Invasive Bladder Cancer (NMIBC) in Ongoing Phase 1 Trial
Clinical Complete Responses Observed in 4 out of 5 Patients in Subset of Patients with Low Grade Disease; Evidence of Bladder Urothelial Field Effect in Non-Target Tumors
Favorable Safety Profile Observed; Only Grade 1 Drug-Related Adverse Events Reported in Less Than 10% of Patients
Aura Hosting Virtual Urologic Oncology Investor Event with Key Opinion Leaders at 4.30 pm ET Today
BOSTON, MA - October 17, 2024 - Aura Biosciences, Inc. (NASDAQ: AURA), today announced positive early data from an ongoing Phase 1 clinical trial of bel-sar (AU-011) in patients with NMIBC. To date, the trial includes 13 patients, with the primary endpoints of evaluating the safety and feasibility of local administration of bel-sar alone (n=5) and bel-sar with light activation (n=8). The secondary endpoints are to evaluate biological activity and immune mediated changes in the tumor microenvironment (TME). 10 of 13 study participants had low grade disease, approximating the 70% incidence of this patient population among all NMIBC patients. The other 3 study participants had high grade disease. In patients receiving bel-sar with light activation (n=8), 4 out of 5 patients with low grade disease demonstrated a clinical complete response with no tumor cells remaining on histopathological evaluation. 2 out of 3 patients with high grade disease demonstrated visual tumor shrinkage observed on cystoscopy. Aura will host a Virtual Urologic Oncology Investor Event at 4:30 pm ET today.
“We are highly encouraged by this positive early data, which shows that bel-sar has the potential to be a transformative cancer treatment,” said Sabine Brookman-May, MD, FEBU, Senior Vice President, Therapeutic Area Head Urologic Oncology of Aura Biosciences. “A potentially differentiating aspect of this novel treatment is the rapid tumor response accompanied by an immune oncology (IO) effect such as a marked CD8+ T-cell infiltration observed in just a matter of days with a single low dose. We believe this could have the potential to translate into a durable response. In parallel with expanding the ongoing Phase 1 trial, we are preparing for a Phase 2 trial to further evaluate bel-sar’s clinical activity and durability of response.”
“Bel-sar has the potential to change the treatment paradigm for NMIBC,” said Neal Shore, MD, FACS, Medical Director, Carolina Urologic Research Center, AUC Urology Specialists. “Based on this early data, bel-sar’s positive clinical activity and evidence of a bladder urothelial field effect with a single dose, may position bel-sar to be the first immune ablative treatment option for early-stage bladder cancer patients delivered with an in-office procedure.”
Bel-sar is a virus-like drug conjugate, designed to have a dual mechanism of action, that induces direct tumor cell necrosis and elicits a robust and durable anti-tumor immune response.
Trial Design: The ongoing Phase 1 trial (NCT05483868) is a two-part, open-label clinical trial, designed to assess the safety and feasibility of bel-sar as a monotherapy. The study treatment is administered 7 to 12 days before the scheduled transurethral resection of bladder tumor (TURBT), the standard of care procedure. The participants are followed for safety monitoring over a 56-day period. The trial is also evaluating bel-sar’s biological activity with histopathological evaluation of tissue samples collected at the time of TURBT (regardless of tumor response) with evaluation of focal necrosis and immune changes in the tumor microenvironment. Part 1 (n=5) of the trial is complete, with patients receiving a single bel-sar dose without light activation. Part 2 (n=10) of the trial is ongoing. 8 patients with a confirmed tumor at time of treatment have received either 100ug or 200ug of bel-sar as a single dose. Of these 8 patients, 5 had low grade disease and 3 had high grade disease. 7 of these 8 patients had a history of recurrent bladder cancer and had undergone multiple TURBTs and adjuvant treatments such as Bacillus Calmette-Guerin (BCG), mitomycin, gemcitabine, cetrelimab and tamoxifen prior to trial enrollment. In the Phase 1 trial expansion, Aura plans to test additional doses and treatment regimens.
Safety Data: In the safety analysis as of the September 9, 2024 data cut-off date (n=12), bel-sar was well-tolerated, with less than 10% of patients reporting Grade 1 and no Grade 2 or higher drug-related adverse events reported. No serious adverse events have been reported. No significant differences between the light-activated and non-light activated cohorts have been observed.
Biological Activity: The data in these 8 patients receiving bel-sar with light activation showed clinical activity detectable as soon as 7 days after a single low dose of bel-sar with light activation. This was demonstrated by histopathological evidence of clinical complete response, necrosis, immune activation or visual tumor shrinkage observed on cystoscopy. For this analysis, “clinical complete response” was defined as the absence of tumor cells on histopathologic evaluation. Of the patients with low-grade disease, 4 out of 5 exhibited a clinical complete response (1 of 4 based on local pathology with central review ongoing), with no tumor cells detected in histopathological evaluation post-treatment in the target and in several non-target bladder tumors. 2 of 3 of the patients with high grade disease demonstrated visual tumor shrinkage observed on cystoscopy, while tumor cells were still present on histopathological evaluation. Immune activation was noted in all patients in both treated target and untreated non-target bladder tumors with infiltration of effector CD8+ and CD4+ T-cells (where immune staining was available). This data provides evidence of a bladder urothelial field effect with a single low dose of bel-sar with light activation, potentially indicating a broader immune response in the bladder beyond the target tumor in these patients.
Aura Virtual Urologic Oncology Investor Event
Aura will host a Virtual Urologic Oncology Investor Event featuring Max Kates, MD (Johns Hopkins), Joe Jacob, MD (Syracuse University), Neal Shore, MD (Carolina Urologic Research Center) and Gary Steinberg, MD (RUSH University) to discuss the early Phase 1 data on Thursday, October 17, 2024, at 4:30 pm Eastern Time. To register for the event, click here. A live question and answer session will follow the formal discussion.
The live webcast of Aura’s Virtual Urologic Oncology Investor Event will be available on the “Investors & Media” page under the “Events & Presentations” section of Aura’s website at https://ir.aurabiosciences.com/events-and-presentations, where a replay of the webcast will be archived for 90 days following the presentation date.
About Aura Biosciences
Aura Biosciences is a clinical-stage biotechnology company focused on developing precision therapies for solid tumors that aim to preserve organ function. Our lead candidate, bel-sar (AU-011), is currently in late-stage development for primary choroidal melanoma and in early-stage development in other ocular oncology indications and bladder cancer. Aura Biosciences is headquartered in Boston, MA. Our mission is to grow as an innovative global oncology company that positively transforms the lives of patients.
For more information, visit aurabiosciences.com. Follow us on X (formerly Twitter) @AuraBiosciences and visit us on LinkedIn.
Forward-Looking Statements
This press release contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995, as amended, and other federal securities laws. Any statements that are not statements of historical fact may be deemed to be forward-looking statements. Words such as “may,” “will,” “could,” “should,” “expects,” “intends,” “plans,” “anticipates,” “believes,” “estimates,” “predicts,” “projects,” “seeks,” “endeavor,” “potential,” “continue” or the negative of such words or other similar expressions can be used to identify forward-looking statements. These forward-looking statements include express or implied statements regarding Aura’s future expectations, plans and prospects, including, without limitation, statements regarding the therapeutic potential of bel-sar for the treatment of cancers including bladder cancer; statements regarding Aura’s plans and expectations for the ongoing Phase 1 and future trials of bel-sar for bladder cancer; statements regarding Aura’s beliefs and expectations for bel-sar’s ability to provide durable responses in bladder cancer patients; statements regarding Aura’s expectations for an improved quality of life of patients after treatment with bel-sar and changes to the treatment paradigm for patients; statements regarding Aura’s beliefs and expectations for the high unmet medical need for an effective local treatment in urologic oncology; and statements regarding Aura’s expectations for the estimated patient populations and related market opportunities for bel-sar.
The forward-looking statements in this press release are neither promises nor guarantees, and investors should not place undue reliance on these forward-looking statements because they involve known and unknown risks, uncertainties and other factors, many of which are beyond Aura’s control and which could cause actual results to differ materially from those expressed or implied by these forward-looking statements, including, without limitation, uncertainties inherent in clinical trials and in the availability and timing of data from ongoing clinical trials; the expected timing for submissions for regulatory approval or review by governmental authorities; the risk that the results of Aura’s preclinical and clinical trials may not be predictive of future results in connection with future clinical trials; the risk that early data from ongoing clinical trials may not be predictive of final data from completed clinical trials; the risk that governmental authorities may disagree with Aura’s clinical trial designs; whether Aura will receive regulatory approvals to conduct trials or to market products; whether Aura’s cash resources will be sufficient to fund its foreseeable and unforeseeable operating expenses and capital expenditure requirements; Aura’s ongoing and planned preclinical activities; and Aura’s ability to initiate, enroll, conduct or complete ongoing and planned clinical trials. These risks, uncertainties and other factors include those risks and uncertainties described under the heading “Risk Factors” in Aura’s most recent Annual Report on Form 10-K and Quarterly Report on Form 10-Q filed with the United States Securities and Exchange Commission (SEC) and in subsequent filings made by Aura with the SEC, which are available on the SEC’s website at www.sec.gov. Except as required by law, Aura disclaims any intention or responsibility for updating or revising any forward-looking statements contained in this press release in the event of new information, future developments or otherwise. These forward-looking statements are based on Aura’s current expectations and speak only as of the date hereof and no representations or warranties (express or implied) are made about the accuracy of any such forward-looking statements.
Investor Contact:
Alex Dasalla
Head of Investor Relations and Corporate Communications
IR@aurabiosciences.com
Media Contact:
Kimberly Ha
KKH Advisors
kimberly.ha@kkhadvisors.com
917-291-5744

Exhibit 99.2 To innovate the future of cancer care to cure patients and preserve organ function October 17, 2024 1
Legal disclosure This presentation contains forward-looking statements, all of which are qualified in their entirety by this cautionary statement. Many of the forward-looking statements contained herein can be identified by the use of forward-looking words such as may , anticipate , believe , could', expect , should , plan , intend , estimate , will , potential and ongoing , among others, although not all forward-looking statements contain these identifying words. These forward-looking statements include statements about the initiation, timing, progress, results and cost of our research and development programs and our current and future preclinical studies and clinical trials, including statements regarding the timing of initiation and completion of studies or trials and related preparatory work, the period during which the results of the trials will become available and our research and development programs; statements regarding our expectations for an improved quality of life of patients after treatment with bel-sar and changes to the treatment paradigm for patients; statements regarding our beliefs and expectations for the high unmet medical need for an effective local treatment in urologic oncology to preserve organ function; and the size and growth potential of the markets for our product candidates and our ability to serve those markets. Except as otherwise noted, these forward-looking statements speak only as of the date of this presentation, and we undertake no obligation to update or revise any of such statements to reflect events or circumstances occurring after this presentation. Because forward-looking statements are inherently subject to risks and uncertainties, some of which cannot be predicted or quantified and some of which are beyond our control, you should not rely on these forward-looking statements as predictions of future events. For a discussion of these and other risks and uncertainties, and other important factors, any of which could cause our actual results to differ from those contained in the forward-looking statements, see the section entitled Risk Factors in our most recent Annual Report on Form 10-K and Quarterly Report on Form 10-Q filed with the Securities and Exchange Commission (SEC), as well as discussions of potential risks, uncertainties, and other important factors in our other subsequent filings with the SEC, which are available on the SEC's website at www.sec.gov. The events and circumstances reflected in our forward-looking statements may not be achieved or occur and actual results could differ materially from those projected in the forward-looking statements. We caution you not to place undue reliance on the forward-looking statements contained in this presentation. This presentation discusses product candidates that are under preclinical or clinical evaluation and that have not yet been approved for marketing by the U.S. Food and Drug Administration (FDA) or any other regulatory authority. Until finalized in a clinical study report, clinical trial data presented herein remain subject to adjustment as a result of clinical site audits and other review processes. No representation is made as to the safety or effectiveness of these product candidates for the use for which such product candidates are being studied. This presentation shall not constitute an offer to sell or the solicitation of an offer to buy, nor shall there be any sale of these securities in any state or other jurisdiction in which such offer, solicitation or sale would be unlawful prior to registration or qualification under the securities laws of any such state or other jurisdiction. 2 2

Urologic oncology key opinion leaders participating on today’s call Neal Shore, MD, FACS Gary Steinberg, MD, Max Kates, MD Joe Jacob, MD, MCR Carolina Urologic Johns Hopkins Syracuse University FACS Research Center RUSH University 3 3
Aura leadership participating on today’s call Sabine Brookman- Elisabet de los Pinos, Jill Hopkins, MD Joseph McQuaid, MD Director, Clinical May, MD PhD Chief Medical Officer Development Urologic SVP, Therapeutic Area Founder and CEO And President of R&D Oncology Head Urologic Oncology 4 4
Cancer cases are predicted to increase by 77% by 2050 as our population ages and 1 grows Large increase in the number of Growing need for function- early-stage cancers requiring preserving, organ-sparing, treatment options with improved local therapies that can benefit-risk profile intercept the course of disease 1. World Health Organization. Global cancer burden growing, amidst mounting need for services. 2024. Available at: Global cancer burden growing, amidst mounting need for services (who.int) [Accessed October 1, 2024]. 5 5 5
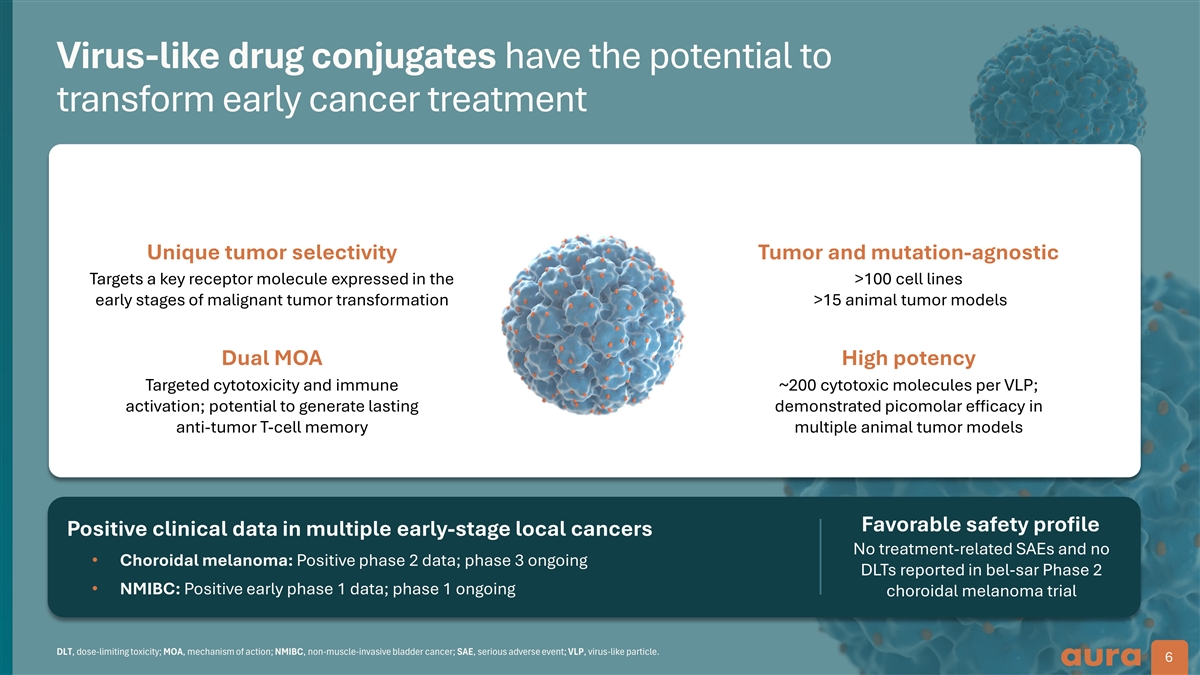
Virus-like drug conjugates have the potential to transform early cancer treatment Unique tumor selectivity Tumor and mutation-agnostic Targets a key receptor molecule expressed in the >100 cell lines early stages of malignant tumor transformation >15 animal tumor models Dual MOA High potency Targeted cytotoxicity and immune ~200 cytotoxic molecules per VLP; activation; potential to generate lasting demonstrated picomolar efficacy in anti-tumor T-cell memory multiple animal tumor models Favorable safety profile Positive clinical data in multiple early-stage local cancers No treatment-related SAEs and no • Choroidal melanoma: Positive phase 2 data; phase 3 ongoing DLTs reported in bel-sar Phase 2 • NMIBC: Positive early phase 1 data; phase 1 ongoing choroidal melanoma trial DLT, dose-limiting toxicity; MOA, mechanism of action; NMIBC, non-muscle-invasive bladder cancer; SAE, serious adverse event; VLP, virus-like particle. 6 6
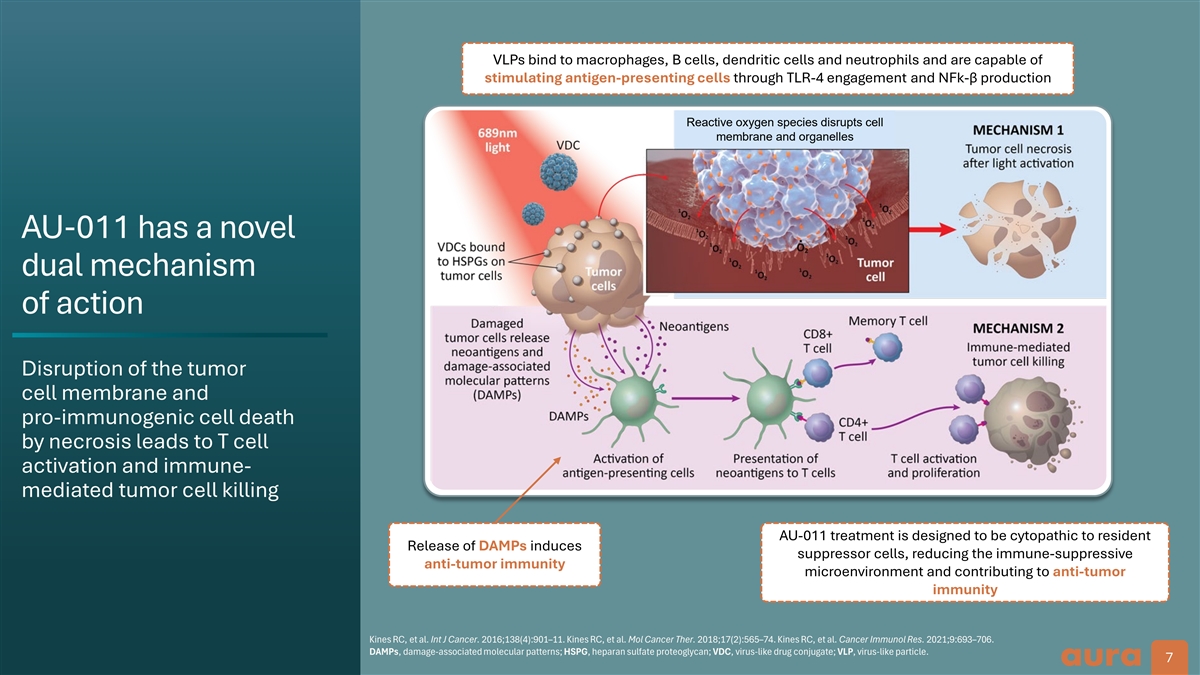
VLPs bind to macrophages, B cells, dendritic cells and neutrophils and are capable of stimulating antigen-presenting cells through TLR-4 engagement and NFk-β production Reactive oxygen species disrupts cell membrane and organelles AU-011 has a novel dual mechanism of action Disruption of the tumor cell membrane and pro-immunogenic cell death by necrosis leads to T cell activation and immune- mediated tumor cell killing AU-011 treatment is designed to be cytopathic to resident Release of DAMPs induces suppressor cells, reducing the immune-suppressive anti-tumor immunity microenvironment and contributing to anti-tumor immunity Kines RC, et al. Int J Cancer. 2016;138(4):901–11. Kines RC, et al. Mol Cancer Ther. 2018;17(2):565–74. Kines RC, et al. Cancer Immunol Res. 2021;9:693–706. DAMPs, damage-associated molecular patterns; HSPG, heparan sulfate proteoglycan; VDC, virus-like drug conjugate; VLP, virus-like particle. 7
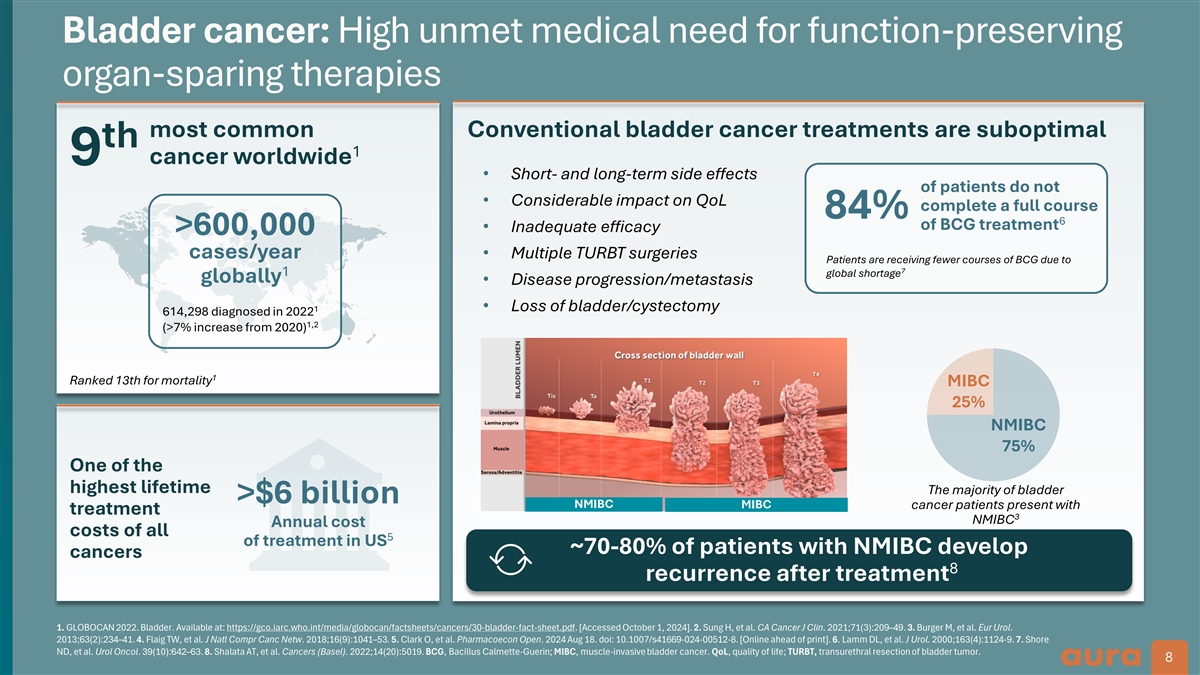
Bladder cancer: High unmet medical need for function-preserving organ-sparing therapies most common Conventional bladder cancer treatments are suboptimal th 1 cancer worldwide 9 • Short- and long-term side effects of patients do not • Considerable impact on QoL complete a full course 84% 6 of BCG treatment • Inadequate efficacy >600,000 cases/year • Multiple TURBT surgeries Patients are receiving fewer courses of BCG due to 7 1 global shortage globally • Disease progression/metastasis • Loss of bladder/cystectomy 1 614,298 diagnosed in 2022 1,2 (>7% increase from 2020) 1 Ranked 13th for mortality MIBC 25% NMIBC 75% One of the highest lifetime The majority of bladder >$6 billion NMIBC MIBC cancer patients present with treatment 3 NMIBC Annual cost costs of all 5 of treatment in US ~70-80% of patients with NMIBC develop cancers 8 recurrence after treatment 1. GLOBOCAN 2022. Bladder. Available at: https://gco.iarc.who.int/media/globocan/factsheets/cancers/30-bladder-fact-sheet.pdf. [Accessed October 1, 2024]. 2. Sung H, et al. CA Cancer J Clin. 2021;71(3):209–49. 3. Burger M, et al. Eur Urol. 2013;63(2):234–41. 4. Flaig TW, et al. J Natl Compr Canc Netw. 2018;16(9):1041–53. 5. Clark O, et al. Pharmacoecon Open. 2024 Aug 18. doi: 10.1007/s41669-024-00512-8. [Online ahead of print]. 6. Lamm DL, et al. J Urol. 2000;163(4):1124-9. 7. Shore ND, et al. Urol Oncol. 39(10):642–63. 8. Shalata AT, et al. Cancers (Basel). 2022;14(20):5019. BCG, Bacillus Calmette-Guerin; MIBC, muscle-invasive bladder cancer. QoL, quality of life; TURBT, transurethral resection of bladder tumor. 8 8 8
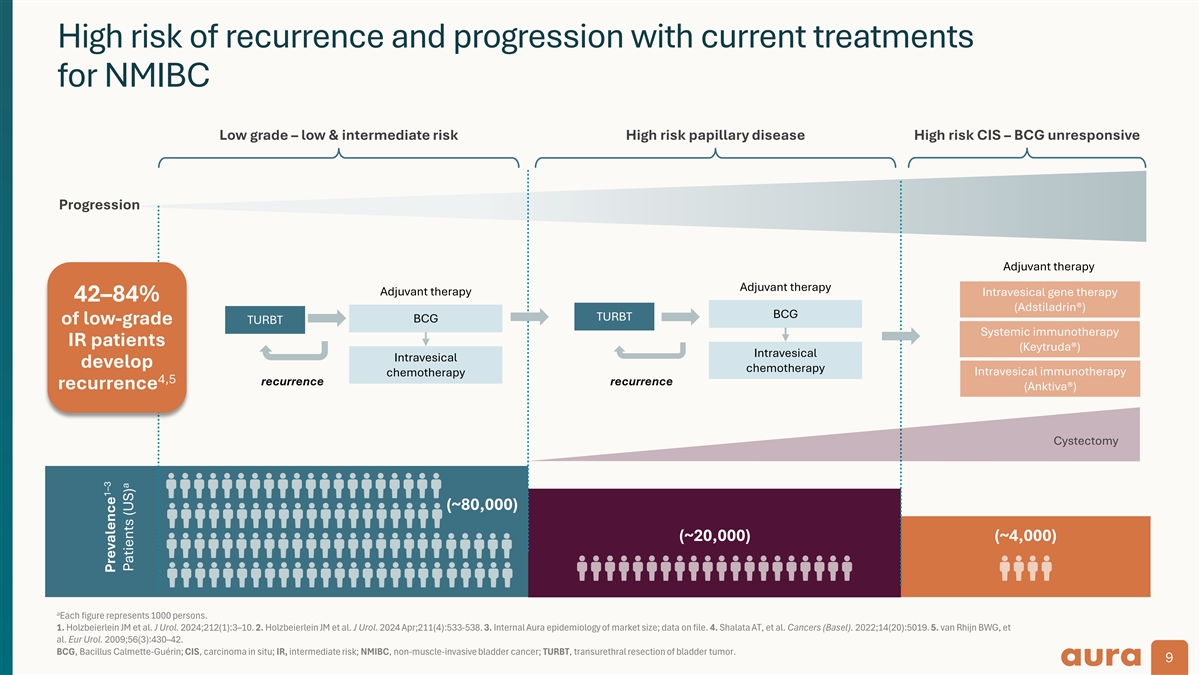
High risk of recurrence and progression with current treatments for NMIBC Low grade – low & intermediate risk High risk papillary disease High risk CIS – BCG unresponsive Progression Adjuvant therapy Adjuvant therapy Adjuvant therapy Intravesical gene therapy 42–84% (Adstiladrin®) BCG TURBT BCG TURBT of low-grade Systemic immunotherapy IR patients (Keytruda®) Intravesical Intravesical develop chemotherapy Intravesical immunotherapy chemotherapy 4,5 recurrence recurrence recurrence (Anktiva®) Cystectomy (~80,000) (~20,000) (~4,000) a Each figure represents 1000 persons. 1. Holzbeierlein JM et al. J Urol. 2024;212(1):3–10. 2. Holzbeierlein JM et al. J Urol. 2024 Apr;211(4):533-538. 3. Internal Aura epidemiology of market size; data on file. 4. Shalata AT, et al. Cancers (Basel). 2022;14(20):5019. 5. van Rhijn BWG, et al. Eur Urol. 2009;56(3):430–42. BCG, Bacillus Calmette-Guérin; CIS, carcinoma in situ; IR, intermediate risk; NMIBC, non-muscle-invasive bladder cancer; TURBT, transurethral resection of bladder tumor. 9 1–3 Prevalence a Patients (US)
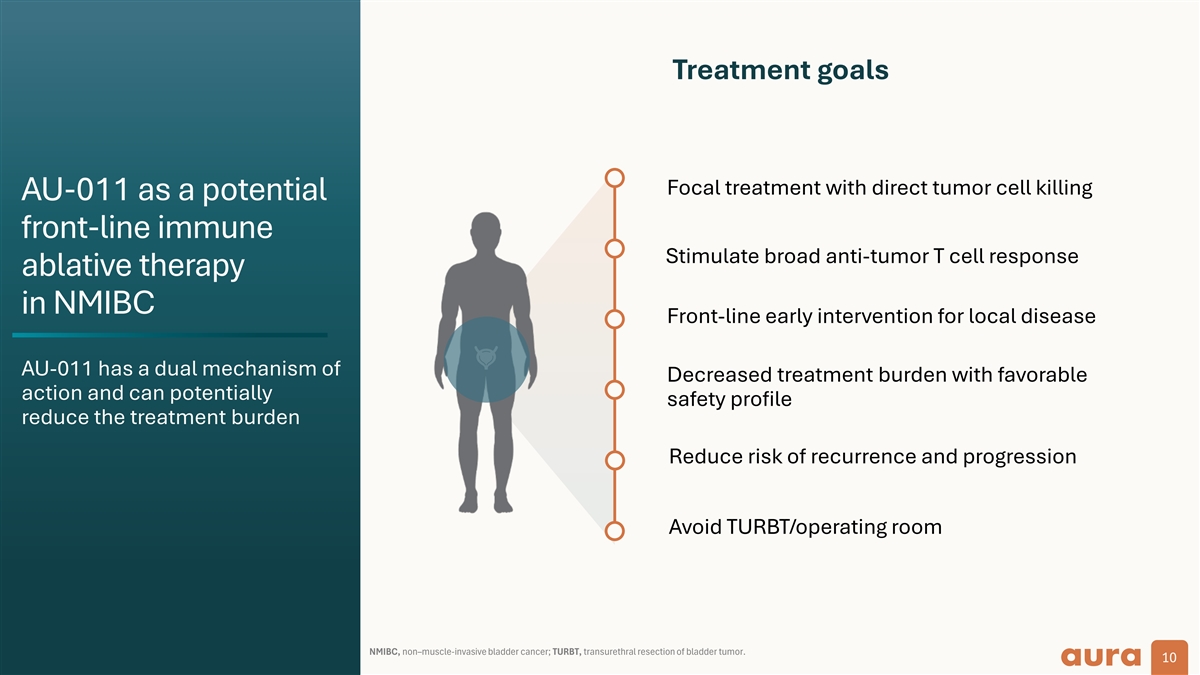
Treatment goals Focal treatment with direct tumor cell killing AU-011 as a potential front-line immune Stimulate broad anti-tumor T cell response ablative therapy in NMIBC Front-line early intervention for local disease AU-011 has a dual mechanism of Decreased treatment burden with favorable action and can potentially safety profile reduce the treatment burden Reduce risk of recurrence and progression Avoid TURBT/operating room NMIBC, non–muscle-invasive bladder cancer; TURBT, transurethral resection of bladder tumor. 10
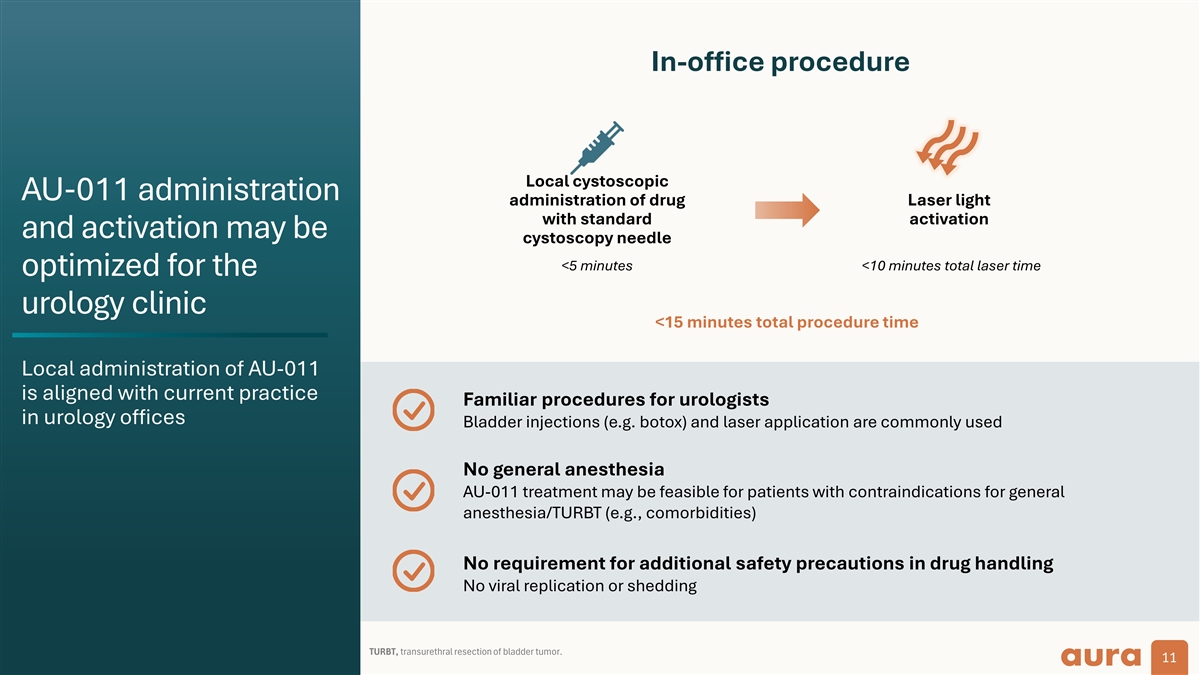
In-office procedure Local cystoscopic AU-011 administration administration of drug Laser light with standard activation and activation may be cystoscopy needle <5 minutes <10 minutes total laser time optimized for the urology clinic <15 minutes total procedure time Local administration of AU-011 is aligned with current practice Familiar procedures for urologists in urology offices Bladder injections (e.g. botox) and laser application are commonly used No general anesthesia AU-011 treatment may be feasible for patients with contraindications for general anesthesia/TURBT (e.g., comorbidities) No requirement for additional safety precautions in drug handling No viral replication or shedding TURBT, transurethral resection of bladder tumor. 11
Phase 1 trial of AU-011 in bladder cancer Review of early data from non-light activated and light-activated NMIBC cohorts
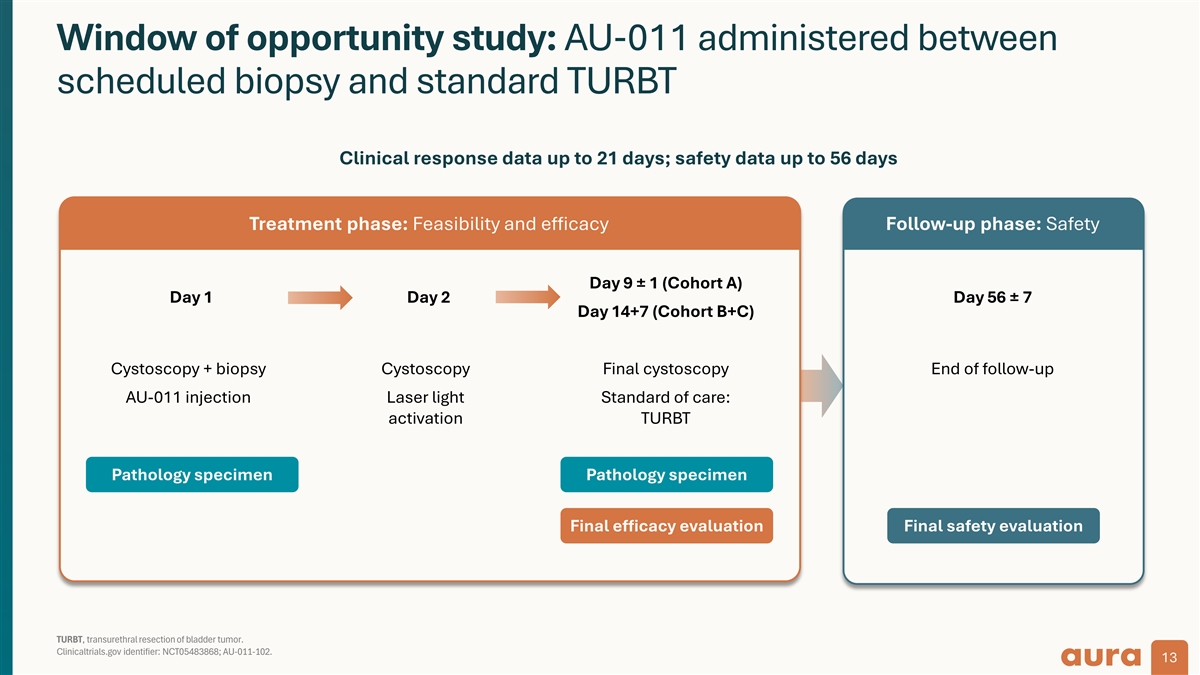
Window of opportunity study: AU-011 administered between scheduled biopsy and standard TURBT Clinical response data up to 21 days; safety data up to 56 days Treatment phase: Feasibility and efficacy Follow-up phase: Safety Day 9 ± 1 (Cohort A) Day 1 Day 2 Day 56 ± 7 Day 14+7 (Cohort B+C) Cystoscopy + biopsy Cystoscopy Final cystoscopy End of follow-up AU-011 injection Laser light Standard of care: activation TURBT Pathology specimen Pathology specimen Final efficacy evaluation Final safety evaluation TURBT, transurethral resection of bladder tumor. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 13
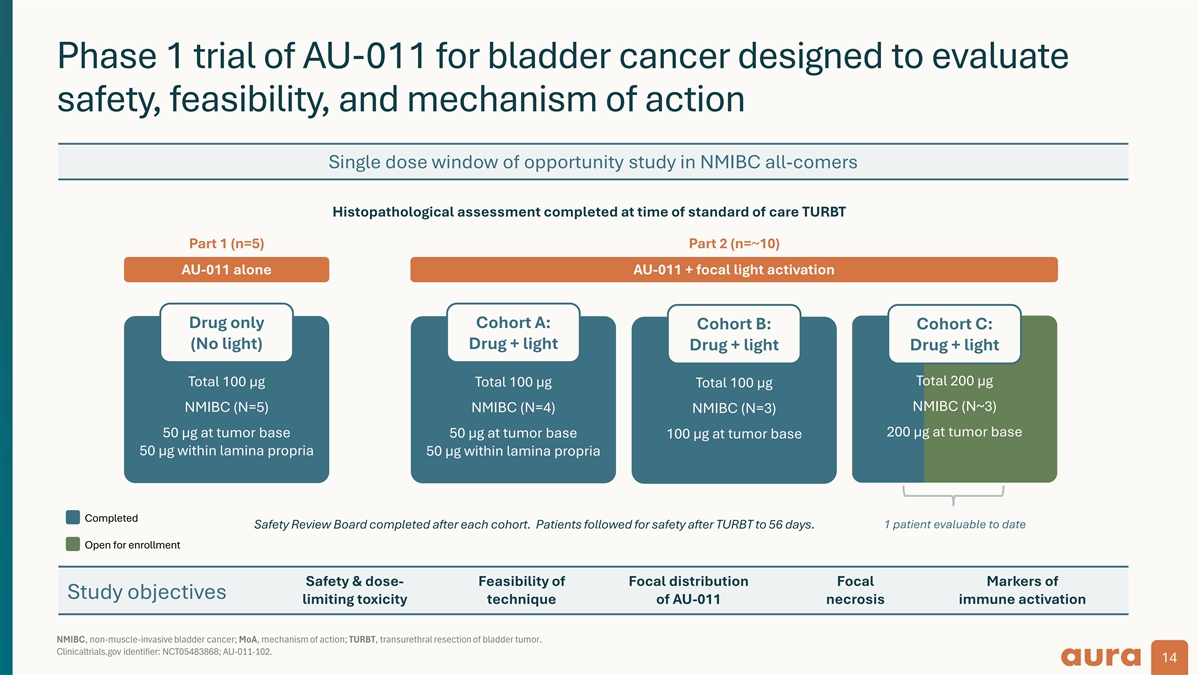
Phase 1 trial of AU-011 for bladder cancer designed to evaluate safety, feasibility, and mechanism of action Single dose window of opportunity study in NMIBC all-comers Histopathological assessment completed at time of standard of care TURBT Part 1 (n=5) Part 2 (n=~10) AU-011 alone AU-011 + focal light activation Drug only Cohort A: Cohort B: Cohort C: (No light) Drug + light Drug + light Drug + light Total 100 µg Total 100 µg Total 200 µg Total 100 µg NMIBC (N~3) NMIBC (N=5) NMIBC (N=4) NMIBC (N=3) 200 µg at tumor base 50 µg at tumor base 50 µg at tumor base 100 µg at tumor base 50 µg within lamina propria 50 µg within lamina propria Completed Safety Review Board completed after each cohort. Patients followed for safety after TURBT to 56 days. 1 patient evaluable to date Open for enrollment Safety & dose- Feasibility of Focal distribution Focal Markers of Study objectives limiting toxicity technique of AU-011 necrosis immune activation NMIBC, non-muscle-invasive bladder cancer; MoA, mechanism of action; TURBT, transurethral resection of bladder tumor. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 14
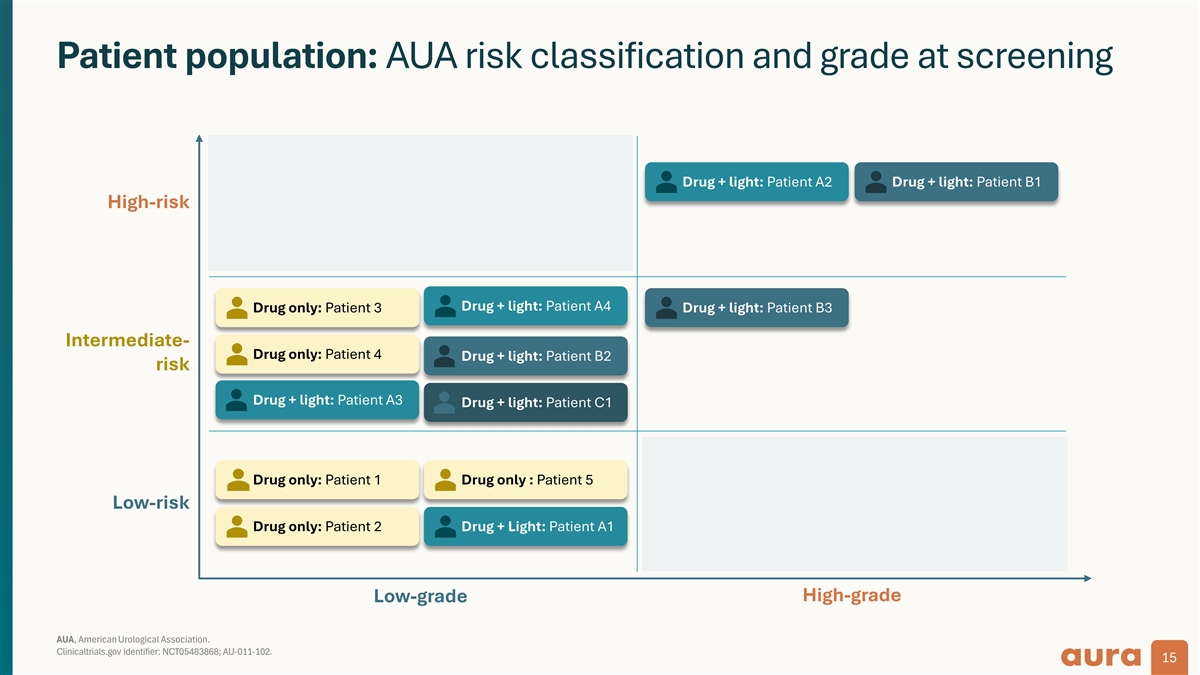
Patient population: AUA risk classification and grade at screening Drug + light: Patient A2 Drug + light: Patient B1 High-risk Drug + light: Patient A4 Drug only: Patient 3 Drug + light: Patient B3 Intermediate- Drug only: Patient 4 Drug + light: Patient B2 risk Drug + light: Patient A3 Drug + light: Patient C1 Drug only: Patient 1 Drug only : Patient 5 Low-risk Drug only: Patient 2 Drug + Light: Patient A1 High-grade Low-grade AUA, American Urological Association. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 15
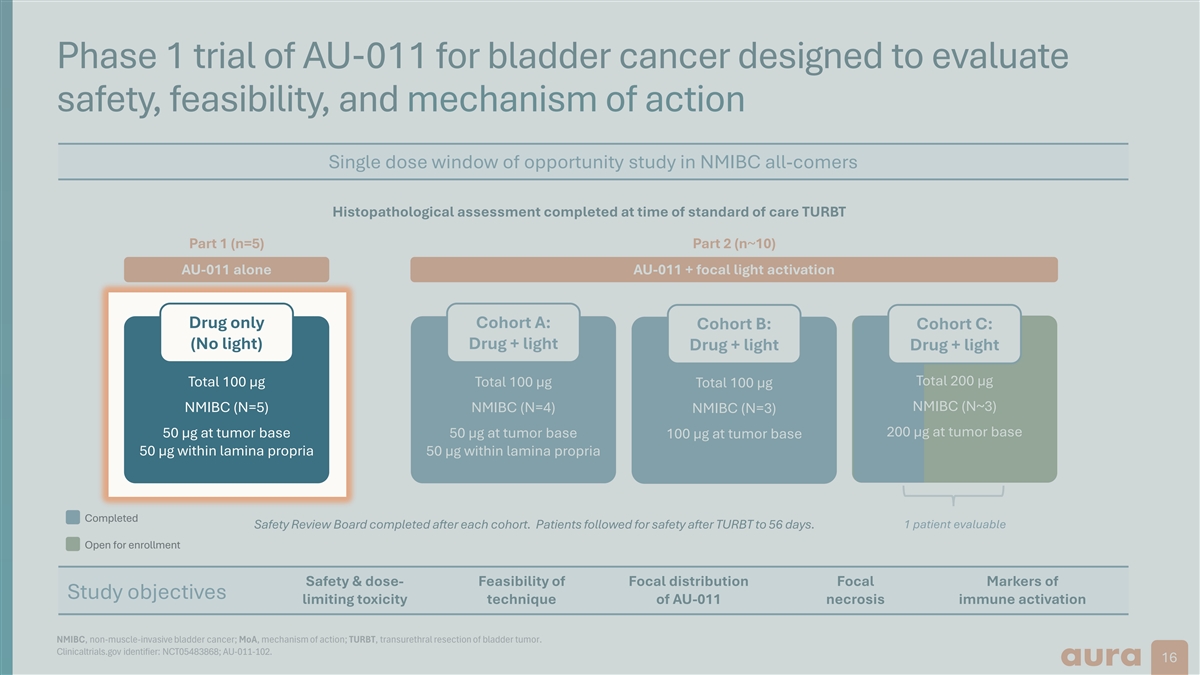
Phase 1 trial of AU-011 for bladder cancer designed to evaluate safety, feasibility, and mechanism of action Single dose window of opportunity study in NMIBC all-comers Histopathological assessment completed at time of standard of care TURBT Part 1 (n=5) Part 2 (n~10) AU-011 alone AU-011 + focal light activation Dr Dru ug o g onl nly y Cohort A: Cohort B: Cohort C: ( (N No o l li ight ght) ) Drug + light Drug + light Drug + light T To ot ta al l 100 µ 100 µg g Total 100 µg Total 200 µg Total 100 µg NMIBC (N~3) N NM MI IBC BC ( (N N=5) =5) NMIBC (N=4) NMIBC (N=3) 200 µg at tumor base 50 µ 50 µg g a at t t tu um mo or r b ba as se e 50 µg at tumor base 100 µg at tumor base 50 µg within lamina propria 50 µg within lamina propria 50 µg within lamina propria Completed Safety Review Board completed after each cohort. Patients followed for safety after TURBT to 56 days. 1 patient evaluable Open for enrollment Safety & dose- Feasibility of Focal distribution Focal Markers of Study objectives limiting toxicity technique of AU-011 necrosis immune activation NMIBC, non-muscle-invasive bladder cancer; MoA, mechanism of action; TURBT, transurethral resection of bladder tumor. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 16
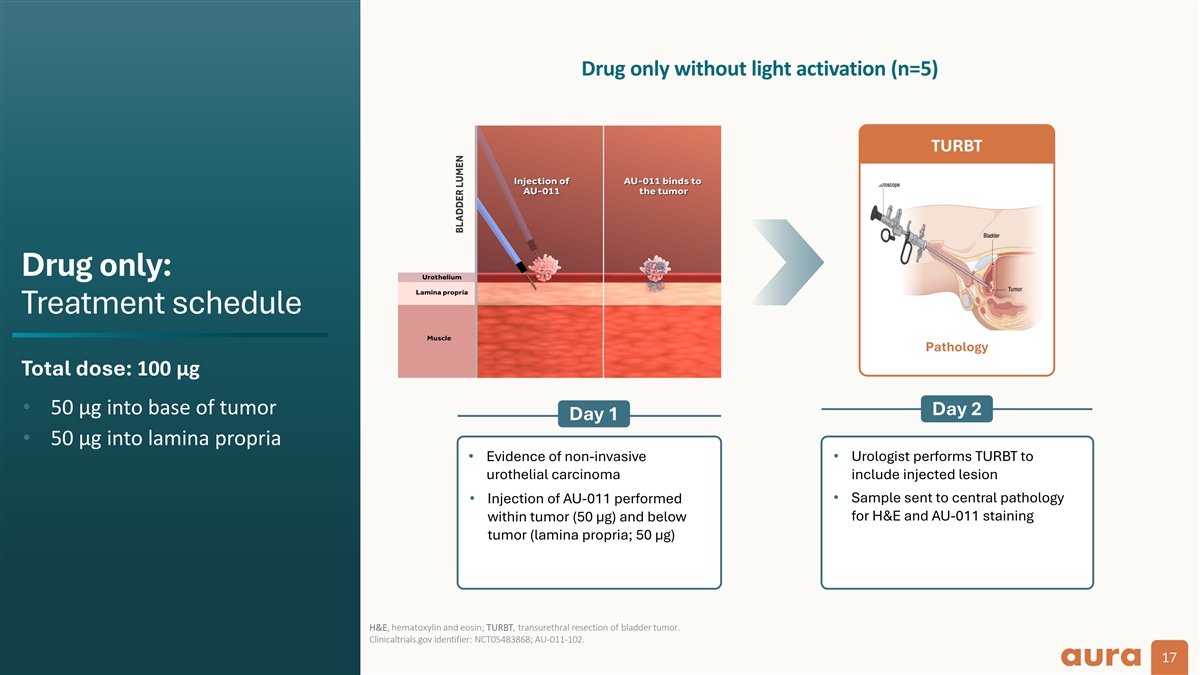
Drug only without light activation (n=5) TURBT Drug only: Treatment schedule Pathology Total dose: 100 µg • 50 µg into base of tumor Day 2 Day 1 • 50 µg into lamina propria • Evidence of non-invasive • Urologist performs TURBT to urothelial carcinoma include injected lesion • Sample sent to central pathology • Injection of AU-011 performed within tumor (50 µg) and below for H&E and AU-011 staining tumor (lamina propria; 50 µg) H&E, hematoxylin and eosin; TURBT, transurethral resection of bladder tumor. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 17
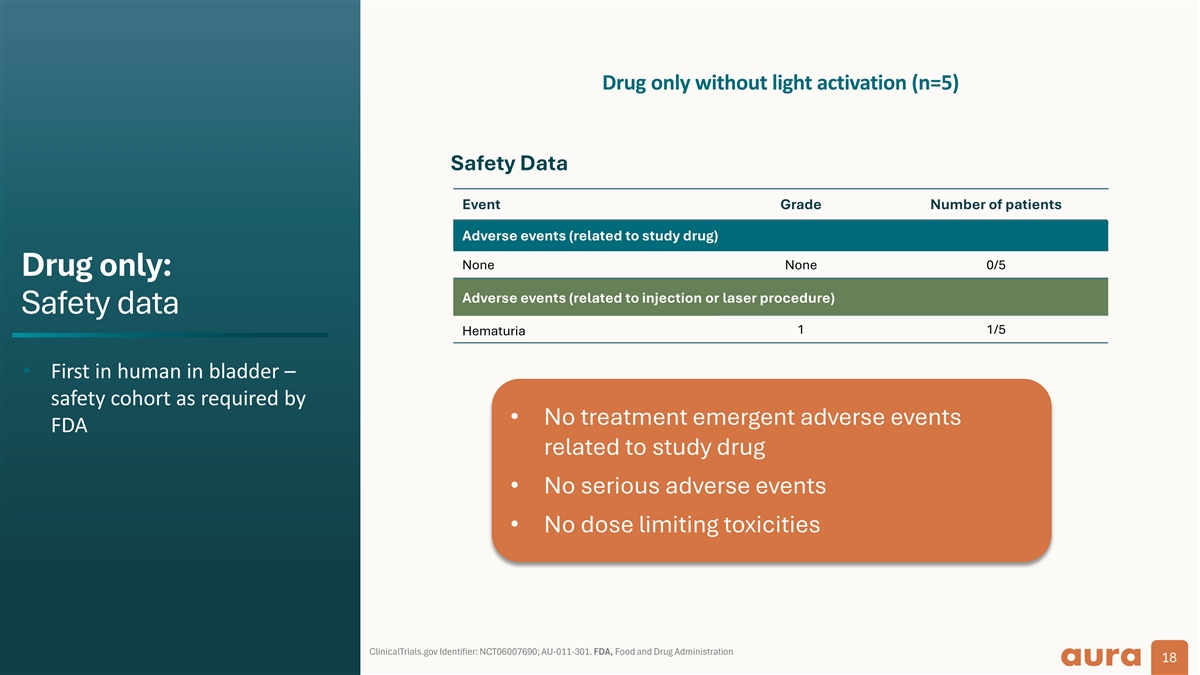
Drug only without light activation (n=5) Safety Data Event Grade Number of patients Adverse events (related to study drug) None None 0/5 Drug only: Adverse events (related to injection or laser procedure) Safety data 1 1/5 Hematuria • First in human in bladder – safety cohort as required by • No treatment emergent adverse events FDA related to study drug • No serious adverse events • No dose limiting toxicities ClinicalTrials.gov Identifier: NCT06007690; AU-011-301. FDA, Food and Drug Administration 18
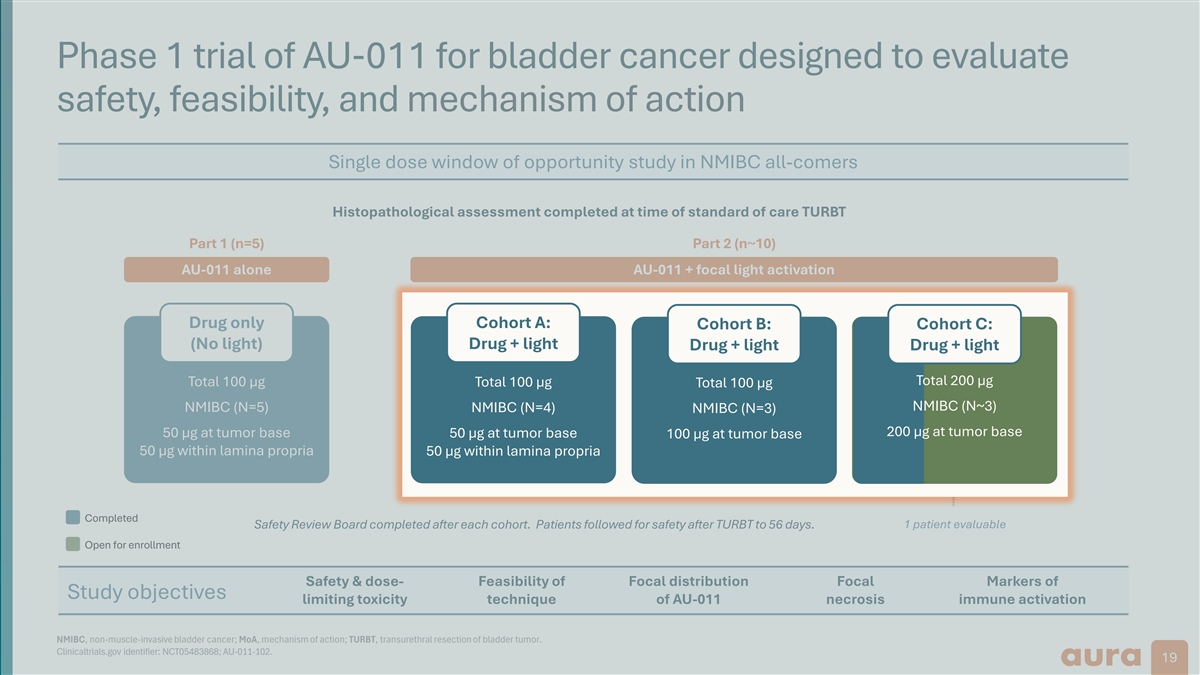
Phase 1 trial of AU-011 for bladder cancer designed to evaluate safety, feasibility, and mechanism of action Single dose window of opportunity study in NMIBC all-comers Histopathological assessment completed at time of standard of care TURBT Part 1 (n=5) Part 2 (n~10) AU-011 alone AU-011 + focal light activation Drug only C Co oh ho ort rt A A: : Cohort C: C Co oh ho ort rt B B: : Cohort C: (No light) Dr Dru ug + g + l li ight ght Drug + light Drug + light Drug + light Drug + light Total 200 µg Total 100 µg Total 100 µg Total 200 µg Total 100 µg T To ot ta al l 100 µ 100 µg g N NMIB MIBC C ( (N N~ ~3) 3) NMIBC (N=5) N NM MI IBC BC ( (N N=4) =4) N NM MI IBC BC ( (N N=3) =3) 20 200 0 µ µg a g at t t tu um mo or b r ba as se e 50 µg at tumor base 50 µ 50 µg g a at t t tu um mo or r b ba as se e 10 100 0 µ µg a g at t t tu um mo or b r ba as se e 50 µg within lamina propria 5 50 0 µ µg g wi wit thi hin l n lam ami ina na pr pro opr pri ia a Completed Safety Review Board completed after each cohort. Patients followed for safety after TURBT to 56 days. 1 patient evaluable Open for enrollment Safety & dose- Feasibility of Focal distribution Focal Markers of Study objectives limiting toxicity technique of AU-011 necrosis immune activation NMIBC, non-muscle-invasive bladder cancer; MoA, mechanism of action; TURBT, transurethral resection of bladder tumor. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 19
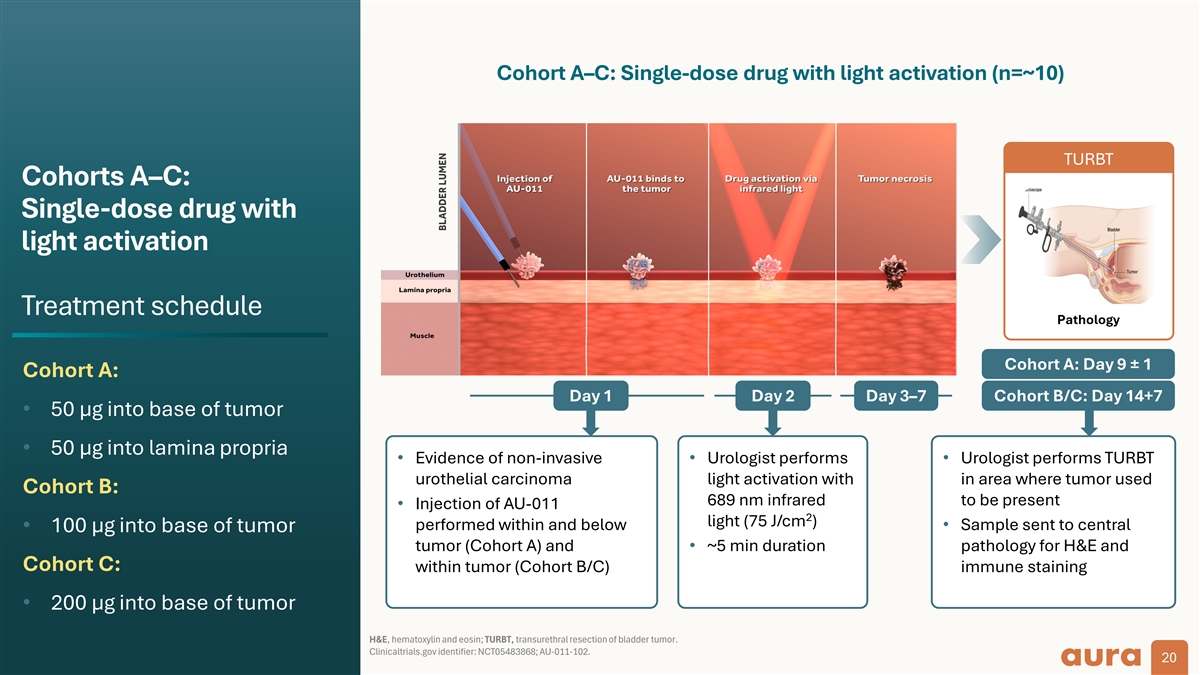
Cohort A–C: Single-dose drug with light activation (n=~10) TURBT Cohorts A–C: Single-dose drug with light activation Treatment schedule Pathology Cohort A: Day 9 ± 1 Cohort A: Day 1 Day 2 Day 3–7 Cohort B/C: Day 14+7 • 50 µg into base of tumor • 50 µg into lamina propria • Evidence of non-invasive • Urologist performs • Urologist performs TURBT urothelial carcinoma light activation with in area where tumor used Cohort B: 689 nm infrared to be present • Injection of AU-011 2 light (75 J/cm ) performed within and below • Sample sent to central • 100 µg into base of tumor tumor (Cohort A) and • ~5 min duration pathology for H&E and Cohort C: within tumor (Cohort B/C) immune staining • 200 µg into base of tumor H&E, hematoxylin and eosin; TURBT, transurethral resection of bladder tumor. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 20
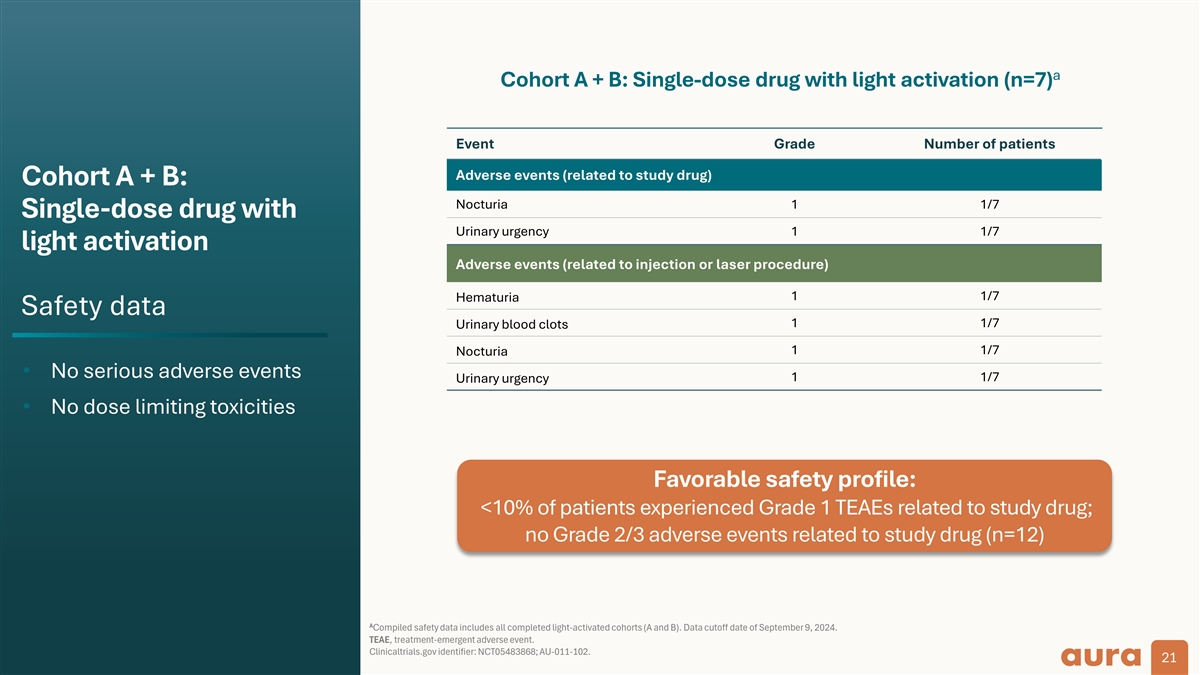
a Cohort A + B: Single-dose drug with light activation (n=7) Event Grade Number of patients Adverse events (related to study drug) Cohort A + B: Nocturia 1 1/7 Single-dose drug with Urinary urgency 1 1/7 light activation Adverse events (related to injection or laser procedure) 1 1/7 Hematuria Safety data 1 1/7 Urinary blood clots 1 1/7 Nocturia • No serious adverse events 1 1/7 Urinary urgency • No dose limiting toxicities Favorable safety profile: <10% of patients experienced Grade 1 TEAEs related to study drug; no Grade 2/3 adverse events related to study drug (n=12) A Compiled safety data includes all completed light-activated cohorts (A and B). Data cutoff date of September 9, 2024. TEAE, treatment-emergent adverse event. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 21
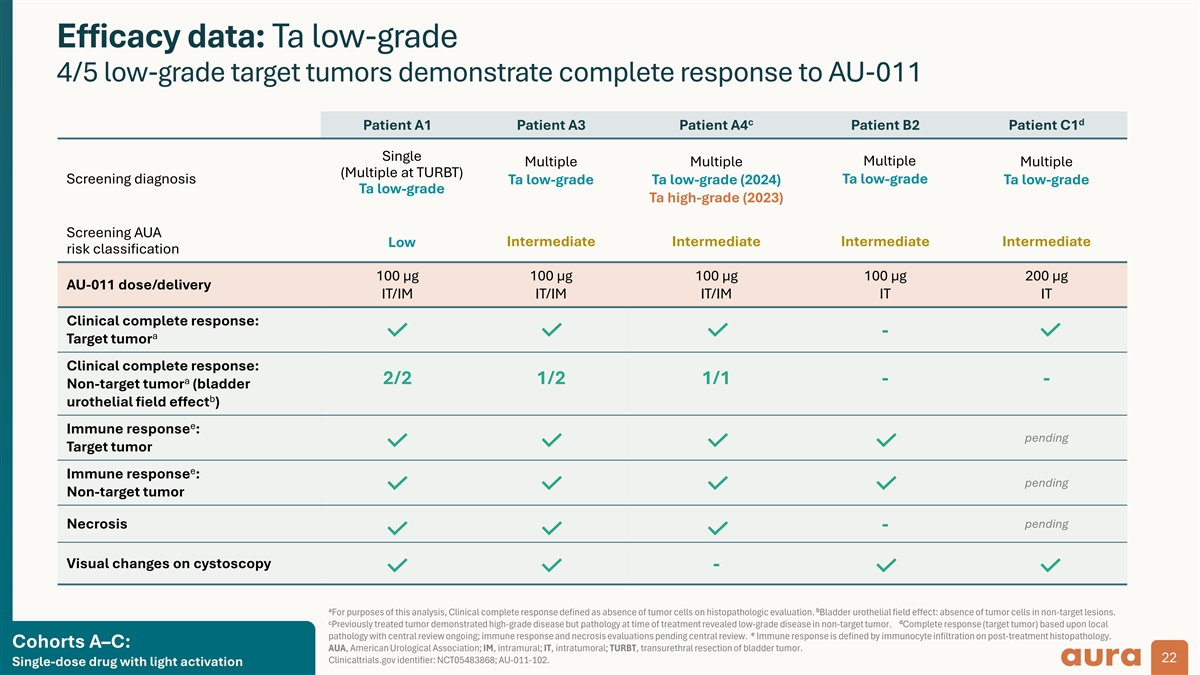
Efficacy data: Ta low-grade 4/5 low-grade target tumors demonstrate complete response to AU-011 c d Patient A1 Patient A3 Patient A4 Patient B2 Patient C1 Single Multiple Multiple Multiple Multiple (Multiple at TURBT) Screening diagnosis Ta low-grade Ta low-grade Ta low-grade (2024) Ta low-grade Ta low-grade Ta high-grade (2023) Screening AUA Intermediate Intermediate Intermediate Intermediate Low risk classification 100 µg 100 µg 100 µg 100 µg 200 µg AU-011 dose/delivery IT/IM IT/IM IT/IM IT IT Clinical complete response: - a Target tumor Clinical complete response: a 2/2 1/2 1/1 - - Non-target tumor (bladder b urothelial field effect ) e Immune response : pending Target tumor e Immune response : pending Non-target tumor pending Necrosis - Visual changes on cystoscopy - a b For purposes of this analysis, Clinical complete response defined as absence of tumor cells on histopathologic evaluation. Bladder urothelial field effect: absence of tumor cells in non-target lesions. C d Previously treated tumor demonstrated high-grade disease but pathology at time of treatment revealed low-grade disease in non-target tumor. Complete response (target tumor) based upon local e pathology with central review ongoing; immune response and necrosis evaluations pending central review. Immune response is defined by immunocyte infiltration on post-treatment histopathology. Cohorts A–C: AUA, American Urological Association; IM, intramural; IT, intratumoral; TURBT, transurethral resection of bladder tumor. 22 Clinicaltrials.gov identifier: NCT05483868; AU-011-102. Single-dose drug with light activation
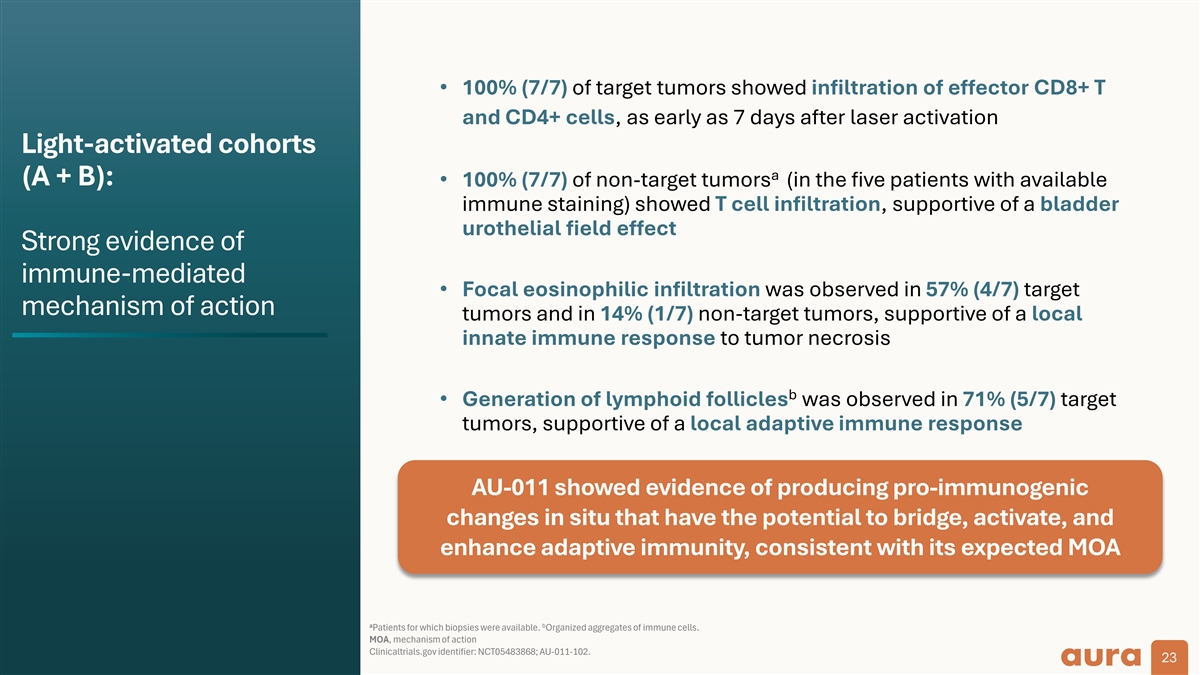
• 100% (7/7) of target tumors showed infiltration of effector CD8+ T and CD4+ cells, as early as 7 days after laser activation Light-activated cohorts a (A + B): • 100% (7/7) of non-target tumors (in the five patients with available immune staining) showed T cell infiltration, supportive of a bladder urothelial field effect Strong evidence of immune-mediated • Focal eosinophilic infiltration was observed in 57% (4/7) target mechanism of action tumors and in 14% (1/7) non-target tumors, supportive of a local innate immune response to tumor necrosis b • Generation of lymphoid follicles was observed in 71% (5/7) target tumors, supportive of a local adaptive immune response AU-011 showed evidence of producing pro-immunogenic changes in situ that have the potential to bridge, activate, and enhance adaptive immunity, consistent with its expected MOA a b Patients for which biopsies were available. Organized aggregates of immune cells. MOA, mechanism of action Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 23
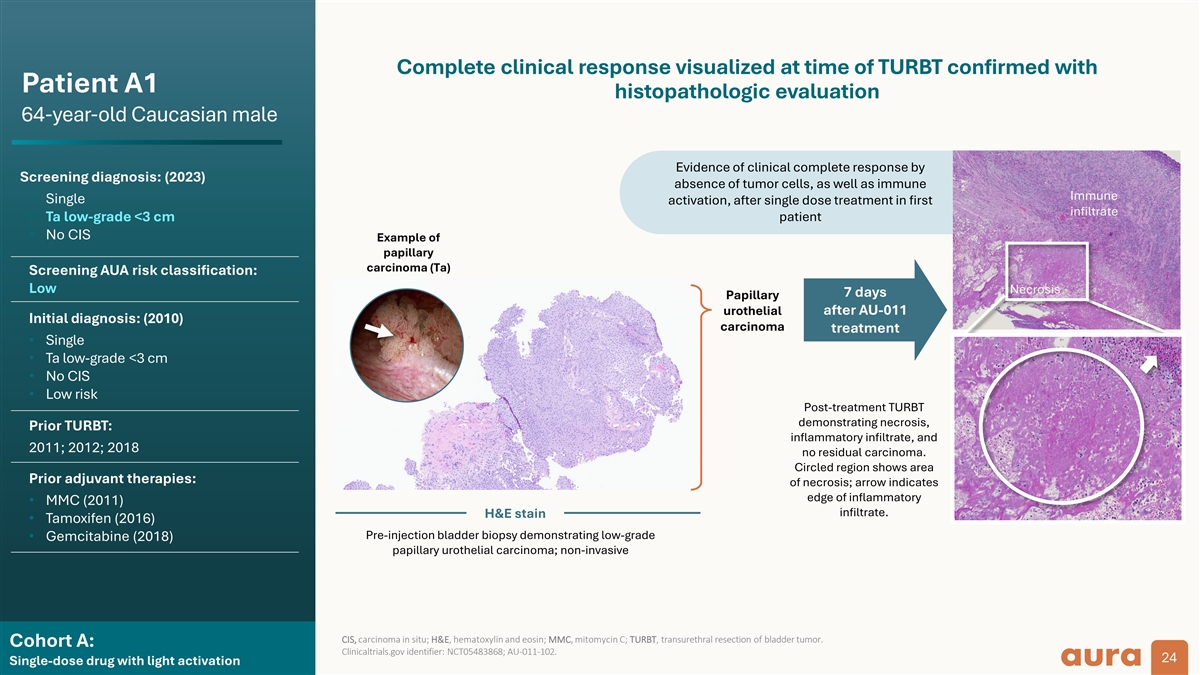
Complete clinical response visualized at time of TURBT confirmed with Patient A1 histopathologic evaluation 64-year-old Caucasian male Evidence of clinical complete response by Screening diagnosis: (2023) absence of tumor cells, as well as immune Immune • Single activation, after single dose treatment in first infiltrate • Ta low-grade <3 cm patient • No CIS Example of papillary carcinoma (Ta) Screening AUA risk classification: Low Necrosis 7 days Papillary urothelial after AU-011 Initial diagnosis: (2010) carcinoma treatment • Single • Ta low-grade <3 cm • No CIS • Low risk Post-treatment TURBT demonstrating necrosis, Prior TURBT: inflammatory infiltrate, and 2011; 2012; 2018 no residual carcinoma. Circled region shows area Prior adjuvant therapies: of necrosis; arrow indicates edge of inflammatory • MMC (2011) infiltrate. H&E stain • Tamoxifen (2016) Pre-injection bladder biopsy demonstrating low-grade • Gemcitabine (2018) papillary urothelial carcinoma; non-invasive CIS, carcinoma in situ; H&E, hematoxylin and eosin; MMC, mitomycin C; TURBT, transurethral resection of bladder tumor. Cohort A: Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 24 Single-dose drug with light activation
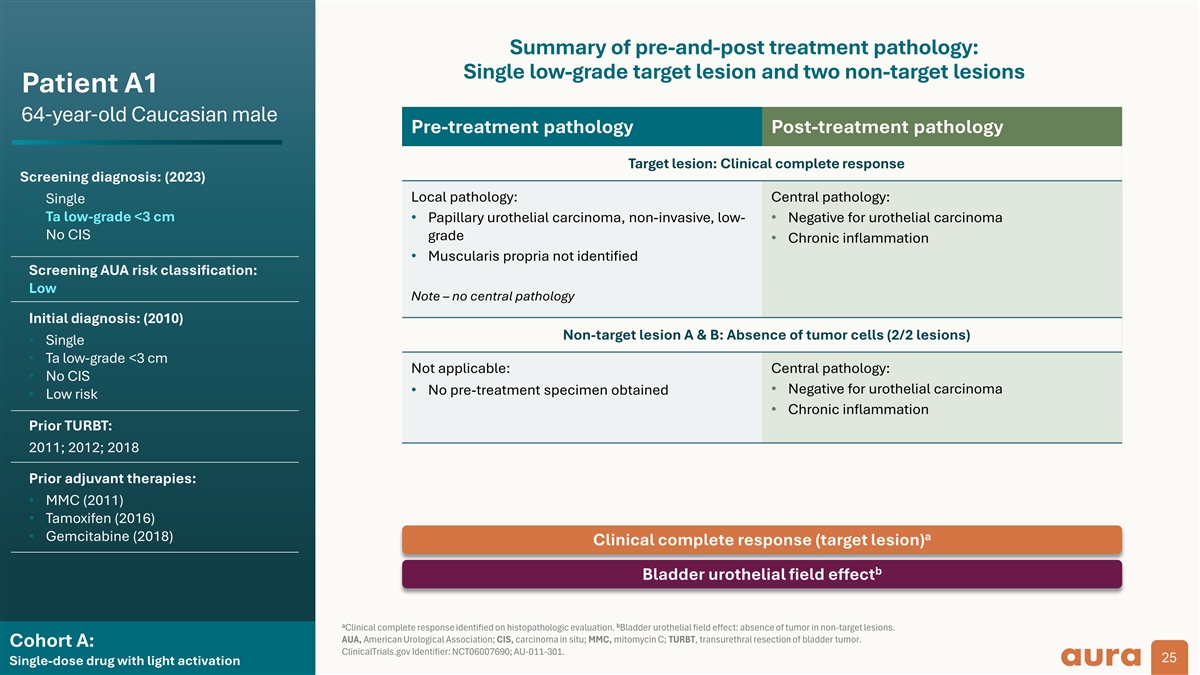
Summary of pre-and-post treatment pathology: Single low-grade target lesion and two non-target lesions Patient A1 64-year-old Caucasian male Pre-treatment pathology Post-treatment pathology Target lesion: Clinical complete response Screening diagnosis: (2023) Local pathology: Central pathology: • Single • Ta low-grade <3 cm • Papillary urothelial carcinoma, non-invasive, low- • Negative for urothelial carcinoma • No CIS grade • Chronic inflammation • Muscularis propria not identified Screening AUA risk classification: Low Note – no central pathology Initial diagnosis: (2010) Non-target lesion A & B: Absence of tumor cells (2/2 lesions) • Single • Ta low-grade <3 cm Not applicable: Central pathology: • No CIS • Negative for urothelial carcinoma • No pre-treatment specimen obtained • Low risk • Chronic inflammation Prior TURBT: 2011; 2012; 2018 Prior adjuvant therapies: • MMC (2011) • Tamoxifen (2016) a • Gemcitabine (2018) Clinical complete response (target lesion) b Bladder urothelial field effect a b Clinical complete response identified on histopathologic evaluation. Bladder urothelial field effect: absence of tumor in non-target lesions. AUA, American Urological Association; CIS, carcinoma in situ; MMC, mitomycin C; TURBT, transurethral resection of bladder tumor. Cohort A: ClinicalTrials.gov Identifier: NCT06007690; AU-011-301. 25 Single-dose drug with light activation
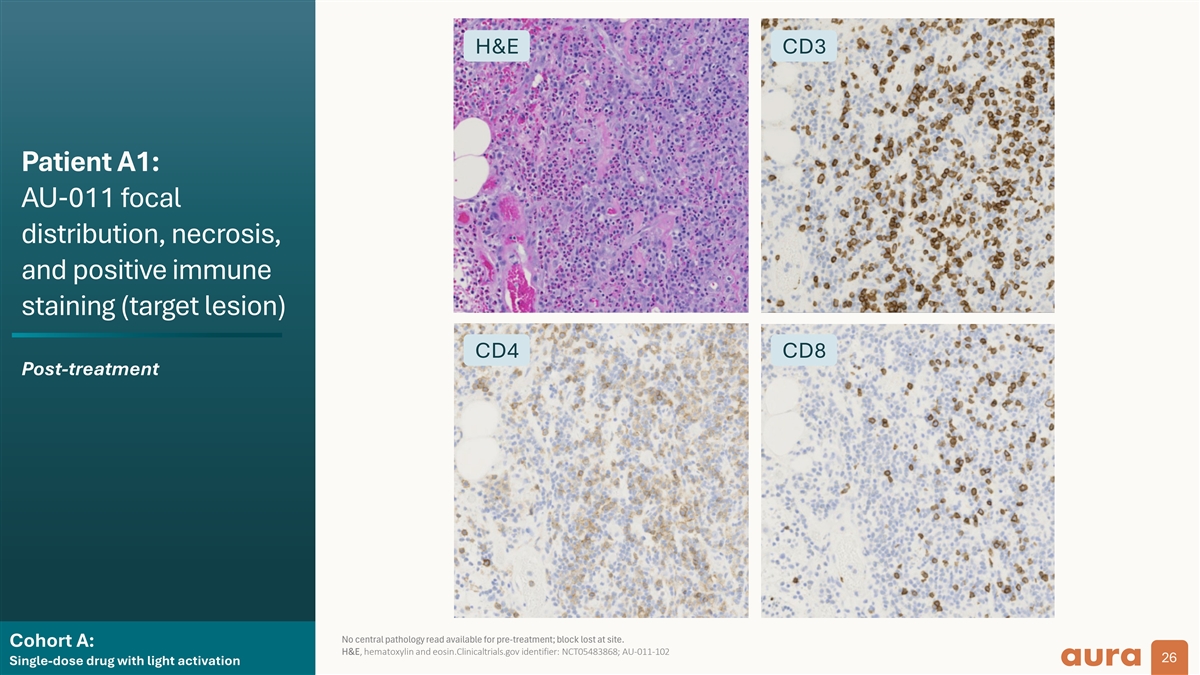
H&E CD3 Patient A1: AU-011 focal distribution, necrosis, and positive immune staining (target lesion) CD4 CD8 Post-treatment No central pathology read available for pre-treatment; block lost at site. Cohort A: H&E, hematoxylin and eosin.Clinicaltrials.gov identifier: NCT05483868; AU-011-102 26 Single-dose drug with light activation
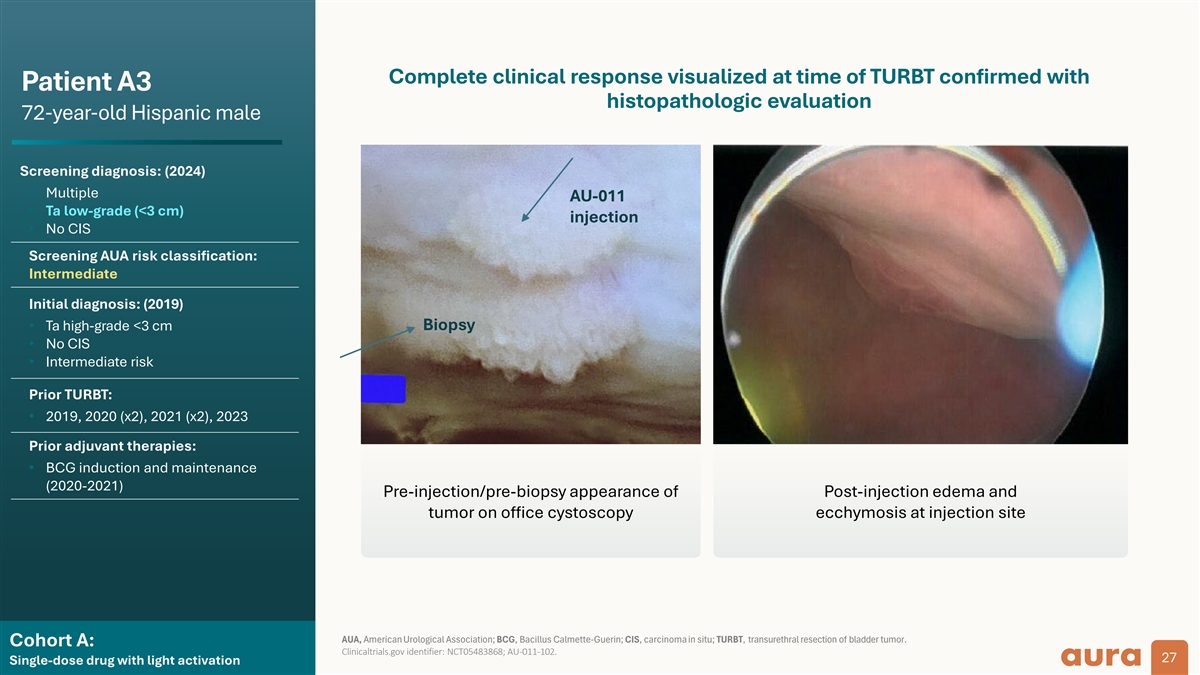
Complete clinical response visualized at time of TURBT confirmed with Patient A3 histopathologic evaluation 72-year-old Hispanic male Screening diagnosis: (2024) • Multiple AU-011 • Ta low-grade (<3 cm) injection • No CIS Screening AUA risk classification: Intermediate Initial diagnosis: (2019) Biopsy • Ta high-grade <3 cm • No CIS • Intermediate risk Prior TURBT: • 2019, 2020 (x2), 2021 (x2), 2023 Prior adjuvant therapies: • BCG induction and maintenance (2020-2021) Pre-injection/pre-biopsy appearance of Post-injection edema and tumor on office cystoscopy ecchymosis at injection site AUA, American Urological Association; BCG, Bacillus Calmette-Guerin; CIS, carcinoma in situ; TURBT, transurethral resection of bladder tumor. Cohort A: Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 27 Single-dose drug with light activation
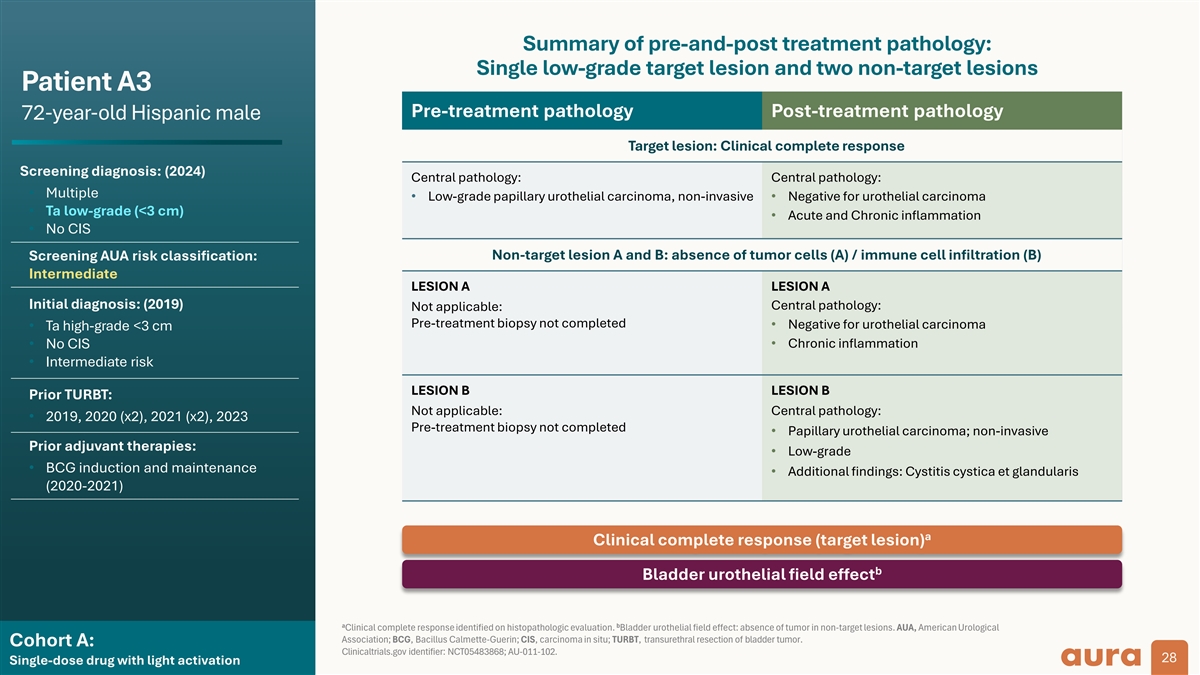
Summary of pre-and-post treatment pathology: Single low-grade target lesion and two non-target lesions Patient A3 Pre-treatment pathology Post-treatment pathology 72-year-old Hispanic male Target lesion: Clinical complete response Screening diagnosis: (2024) Central pathology: Central pathology: • Multiple • Low-grade papillary urothelial carcinoma, non-invasive • Negative for urothelial carcinoma • Ta low-grade (<3 cm) • Acute and Chronic inflammation • No CIS Non-target lesion A and B: absence of tumor cells (A) / immune cell infiltration (B) Screening AUA risk classification: Intermediate LESION A LESION A Initial diagnosis: (2019) Central pathology: Not applicable: Pre-treatment biopsy not completed • Negative for urothelial carcinoma • Ta high-grade <3 cm • Chronic inflammation • No CIS • Intermediate risk LESION B LESION B Prior TURBT: Not applicable: Central pathology: • 2019, 2020 (x2), 2021 (x2), 2023 Pre-treatment biopsy not completed • Papillary urothelial carcinoma; non-invasive Prior adjuvant therapies: • Low-grade • BCG induction and maintenance • Additional findings: Cystitis cystica et glandularis (2020-2021) a Clinical complete response (target lesion) b Bladder urothelial field effect a b Clinical complete response identified on histopathologic evaluation. Bladder urothelial field effect: absence of tumor in non-target lesions. AUA, American Urological Association; BCG, Bacillus Calmette-Guerin; CIS, carcinoma in situ; TURBT, transurethral resection of bladder tumor. Cohort A: Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 28 Single-dose drug with light activation
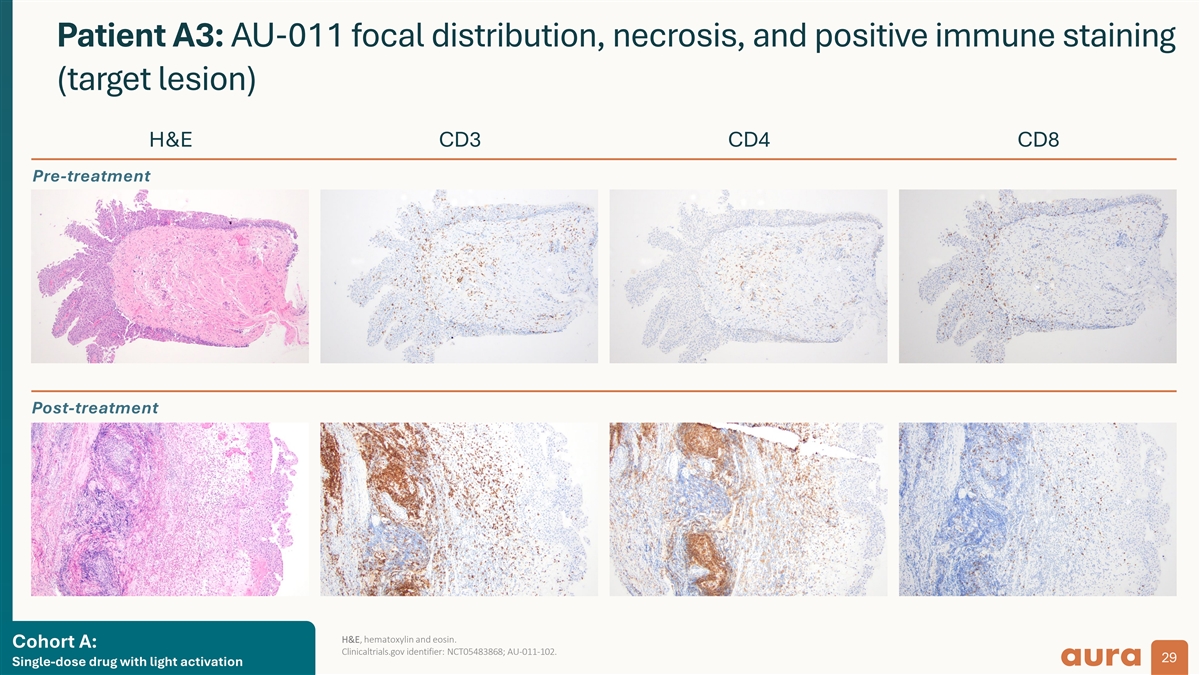
Patient A3: AU-011 focal distribution, necrosis, and positive immune staining (target lesion) H&E CD3 CD4 CD8 Pre-treatment Post-treatment H&E, hematoxylin and eosin. Cohort A: Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 29 Single-dose drug with light activation
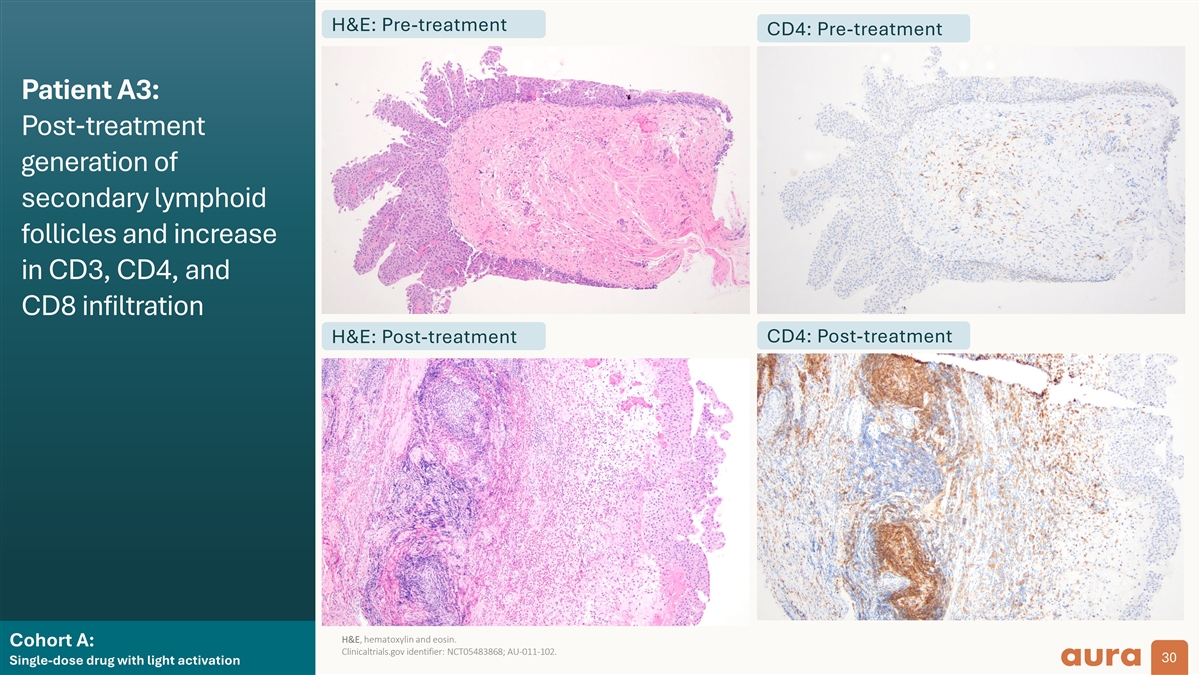
H&E: Pre-treatment CD4: Pre-treatment Patient A3: Post-treatment generation of secondary lymphoid follicles and increase in CD3, CD4, and CD8 infiltration CD4: Post-treatment H&E: Post-treatment H&E, hematoxylin and eosin. Cohort A: Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 30 Single-dose drug with light activation
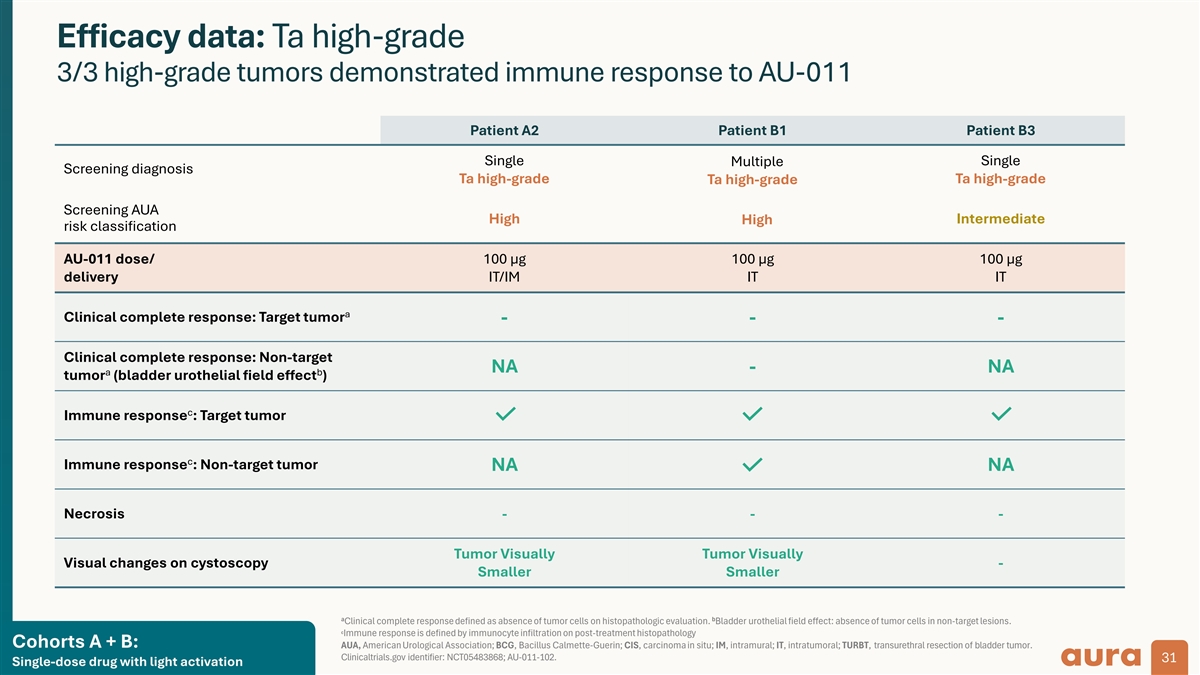
Efficacy data: Ta high-grade 3/3 high-grade tumors demonstrated immune response to AU-011 Patient A2 Patient B1 Patient B3 Single Single Multiple Screening diagnosis Ta high-grade Ta high-grade Ta high-grade Screening AUA High Intermediate High risk classification AU-011 dose/ 100 µg 100 µg 100 µg delivery IT/IM IT IT a Clinical complete response: Target tumor - - - Clinical complete response: Non-target NA - NA a b tumor (bladder urothelial field effect ) c Immune response : Target tumor c Immune response : Non-target tumor NA NA Necrosis - - - Tumor Visually Tumor Visually Visual changes on cystoscopy - Smaller Smaller a b Clinical complete response defined as absence of tumor cells on histopathologic evaluation. Bladder urothelial field effect: absence of tumor cells in non-target lesions. c Immune response is defined by immunocyte infiltration on post-treatment histopathology Cohorts A + B: AUA, American Urological Association; BCG, Bacillus Calmette-Guerin; CIS, carcinoma in situ; IM, intramural; IT, intratumoral; TURBT, transurethral resection of bladder tumor. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 31 Single-dose drug with light activation

Summary
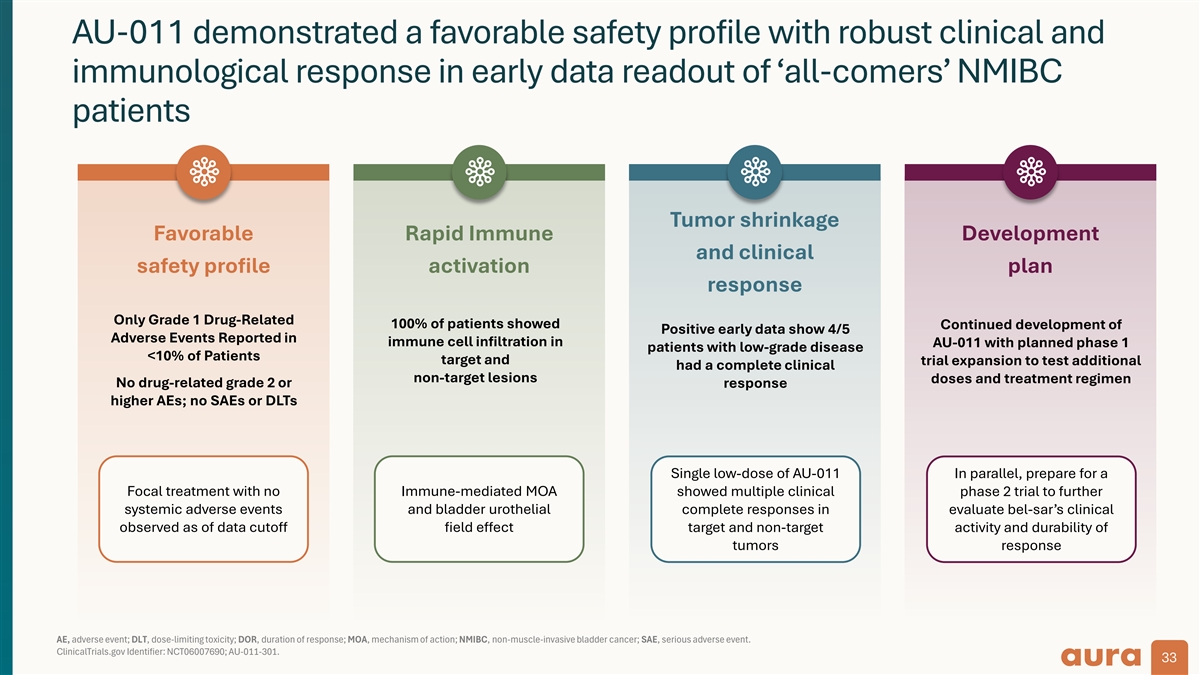
AU-011 demonstrated a favorable safety profile with robust clinical and immunological response in early data readout of ‘all-comers’ NMIBC patients Tumor shrinkage Favorable Rapid Immune Development and clinical safety profile activation plan response Only Grade 1 Drug-Related 100% of patients showed Continued development of Positive early data show 4/5 Adverse Events Reported in immune cell infiltration in AU-011 with planned phase 1 patients with low-grade disease <10% of Patients target and trial expansion to test additional had a complete clinical non-target lesions doses and treatment regimen No drug-related grade 2 or response higher AEs; no SAEs or DLTs Single low-dose of AU-011 In parallel, prepare for a Focal treatment with no Immune-mediated MOA showed multiple clinical phase 2 trial to further systemic adverse events and bladder urothelial complete responses in evaluate bel-sar’s clinical observed as of data cutoff field effect target and non-target activity and durability of tumors response AE, adverse event; DLT, dose-limiting toxicity; DOR, duration of response; MOA, mechanism of action; NMIBC, non-muscle-invasive bladder cancer; SAE, serious adverse event. ClinicalTrials.gov Identifier: NCT06007690; AU-011-301. 33

Appendix

Anti-tumor immunity: Treating beyond the target Preclinical development
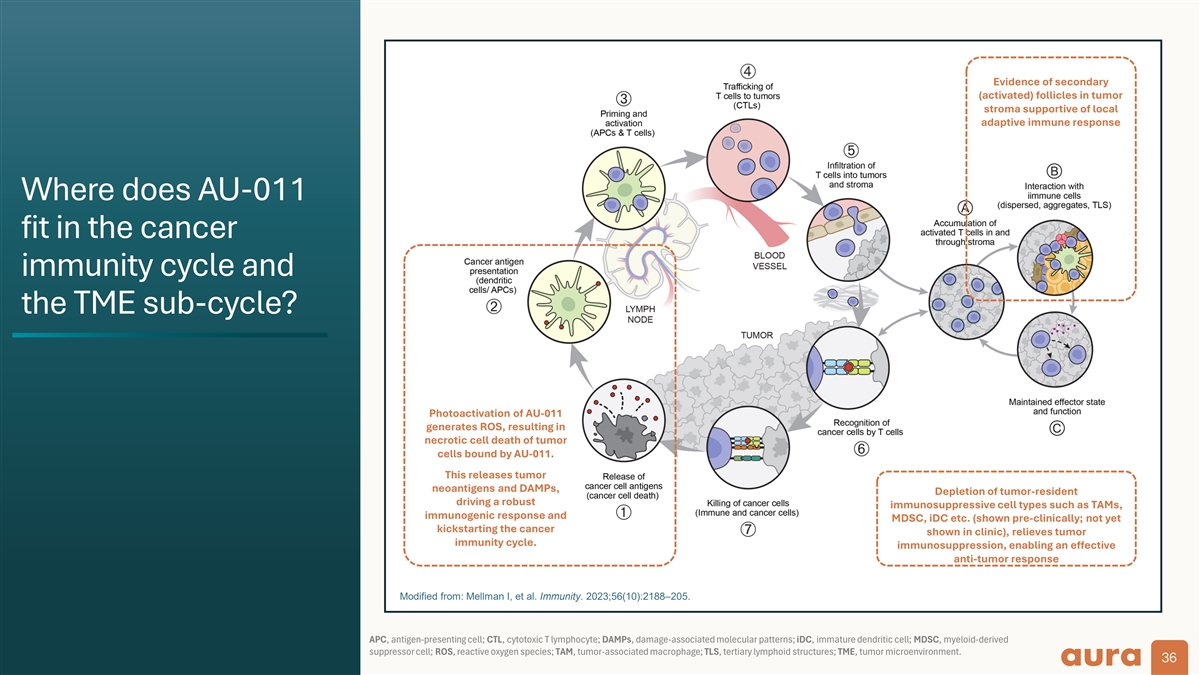
Evidence of secondary (activated) follicles in tumor stroma supportive of local adaptive immune response Where does AU-011 fit in the cancer immunity cycle and the TME sub-cycle? Photoactivation of AU-011 generates ROS, resulting in necrotic cell death of tumor cells bound by AU-011. This releases tumor neoantigens and DAMPs, Depletion of tumor-resident driving a robust immunosuppressive cell types such as TAMs, immunogenic response and MDSC, iDC etc. (shown pre-clinically; not yet kickstarting the cancer shown in clinic), relieves tumor immunity cycle. immunosuppression, enabling an effective anti-tumor response Modified from: Mellman I, et al. Immunity. 2023;56(10):2188–205. APC, antigen-presenting cell; CTL, cytotoxic T lymphocyte; DAMPs, damage-associated molecular patterns; iDC, immature dendritic cell; MDSC, myeloid-derived suppressor cell; ROS, reactive oxygen species; TAM, tumor-associated macrophage; TLS, tertiary lymphoid structures; TME, tumor microenvironment. 36
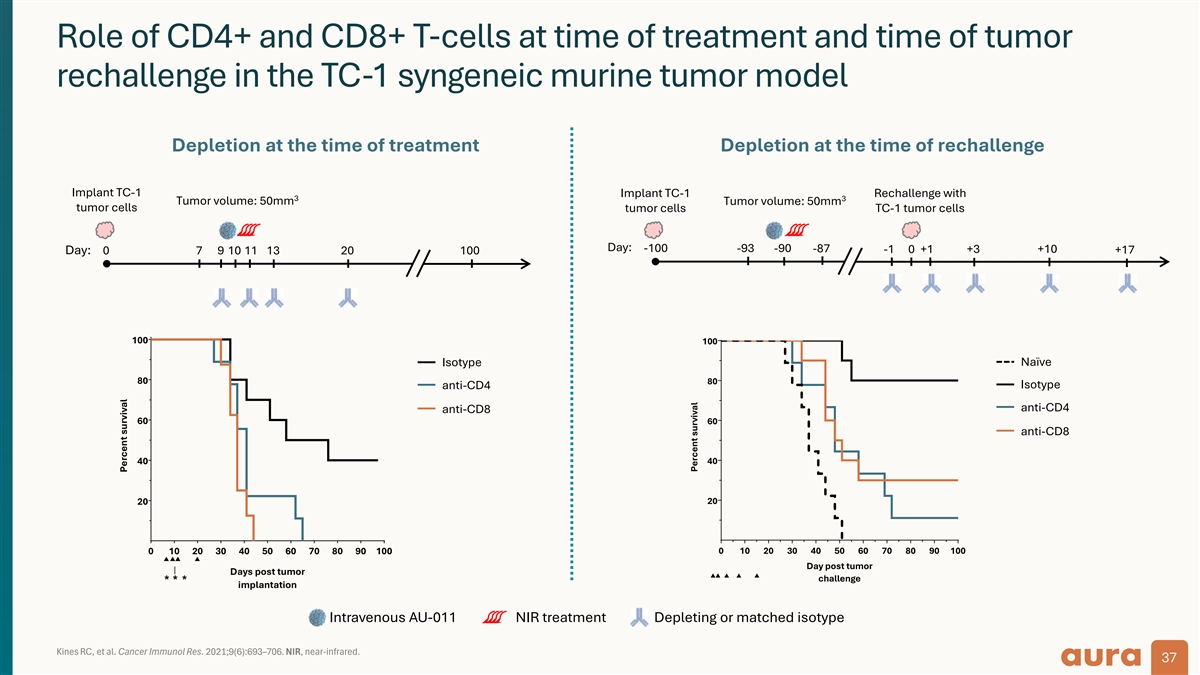
Role of CD4+ and CD8+ T-cells at time of treatment and time of tumor rechallenge in the TC-1 syngeneic murine tumor model Depletion at the time of treatment Depletion at the time of rechallenge Implant TC-1 Implant TC-1 Rechallenge with 3 3 Tumor volume: 50mm Tumor volume: 50mm tumor cells tumor cells TC-1 tumor cells Day: -100 -93 -90 -87 +10 -1 0 +1 +3 +17 Day: 0 7 9 10 11 13 20 100 100 100 Isotype Naïve 80 80 Isotype anti-CD4 anti-CD4 anti-CD8 60 60 anti-CD8 40 40 20 20 0 10 20 30 40 50 60 70 80 90 100 0 10 20 30 40 50 60 70 80 90 100 ▲▲▲▲ Day post tumor Days post tumor ▲▲▲▲▲ challenge * * * implantation Intravenous AU-011 NIR treatment Depleting or matched isotype Kines RC, et al. Cancer Immunol Res. 2021;9(6):693–706. NIR, near-infrared. 37 Percent survival Percent survival
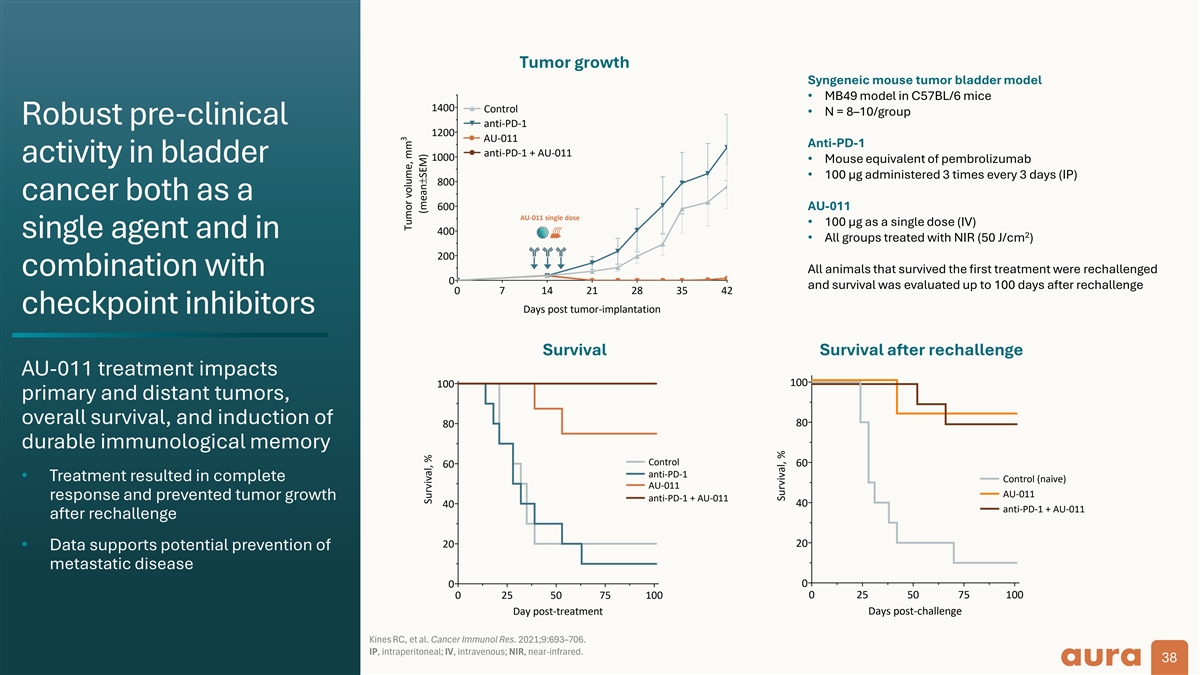
Tumor growth Syngeneic mouse tumor bladder model • MB49 model in C57BL/6 mice 1400 Control • N = 8–10/group Robust pre-clinical anti-PD-1 1200 AU-011 Anti-PD-1 anti-PD-1 + AU-011 1000 activity in bladder • Mouse equivalent of pembrolizumab • 100 µg administered 3 times every 3 days (IP) 800 cancer both as a 600 AU-011 AU-011 single dose • 100 µg as a single dose (IV) 400 2 single agent and in • All groups treated with NIR (50 J/cm ) 200 All animals that survived the first treatment were rechallenged combination with 0 and survival was evaluated up to 100 days after rechallenge 0 7 14 21 28 35 42 Days post tumor-implantation checkpoint inhibitors Survival Survival after rechallenge AU-011 treatment impacts 100 100 primary and distant tumors, overall survival, and induction of 80 80 durable immunological memory Control 60 60 anti-PD-1 • Treatment resulted in complete Control (naive) AU-011 AU-011 response and prevented tumor growth anti-PD-1 + AU-011 40 40 anti-PD-1 + AU-011 after rechallenge 20 20 • Data supports potential prevention of metastatic disease 0 0 0 25 50 75 100 0 25 50 75 100 Day post-treatment Days post-challenge Kines RC, et al. Cancer Immunol Res. 2021;9:693–706. IP, intraperitoneal; IV, intravenous; NIR, near-infrared. 38 3 Tumor volume, mm (mean±SEM) Survival, % Survival, %
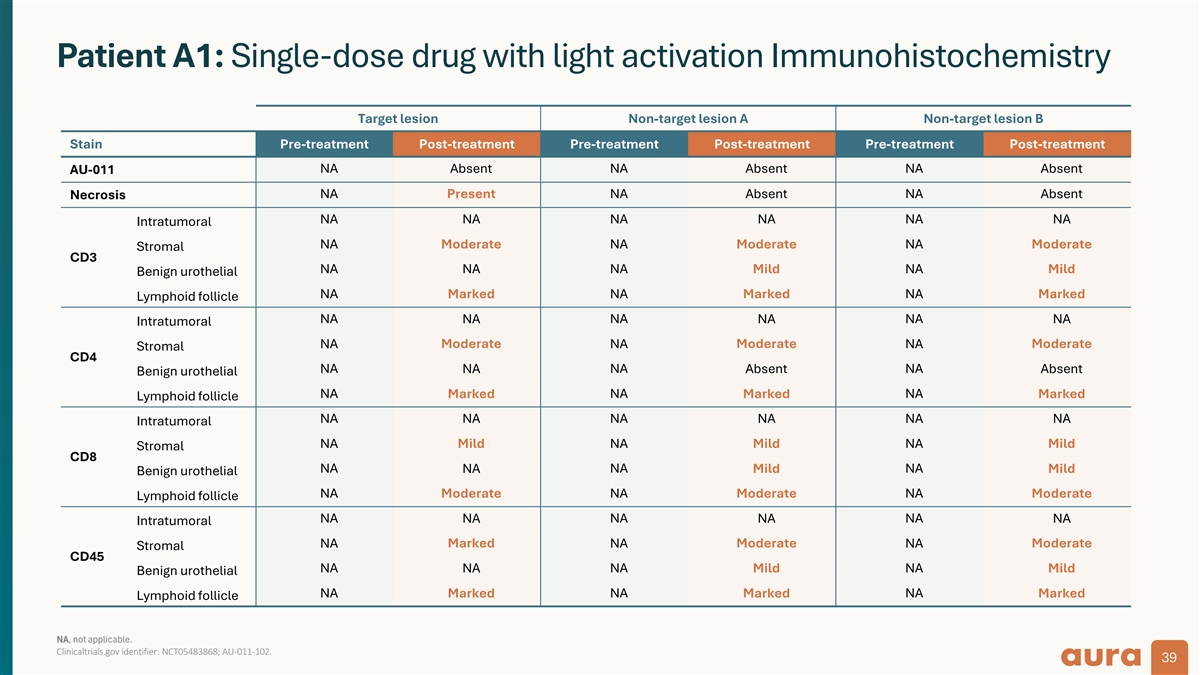
Patient A1: Single-dose drug with light activation Immunohistochemistry Target lesion Non-target lesion A Non-target lesion B Stain Pre-treatment Post-treatment Pre-treatment Post-treatment Pre-treatment Post-treatment NA Absent NA Absent NA Absent AU-011 NA Present NA Absent NA Absent Necrosis NA NA NA NA NA NA Intratumoral NA Moderate NA Moderate NA Moderate Stromal CD3 NA NA NA Mild NA Mild Benign urothelial NA Marked NA Marked NA Marked Lymphoid follicle NA NA NA NA NA NA Intratumoral NA Moderate NA Moderate NA Moderate Stromal CD4 NA NA NA Absent NA Absent Benign urothelial NA Marked NA Marked NA Marked Lymphoid follicle NA NA NA NA NA NA Intratumoral Mild Mild Mild NA NA NA Stromal CD8 NA NA NA NA Mild Mild Benign urothelial NA Moderate NA Moderate NA Moderate Lymphoid follicle NA NA NA NA NA NA Intratumoral NA Marked NA Moderate NA Moderate Stromal CD45 NA NA NA Mild NA Mild Benign urothelial NA Marked NA Marked NA Marked Lymphoid follicle NA, not applicable. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 39
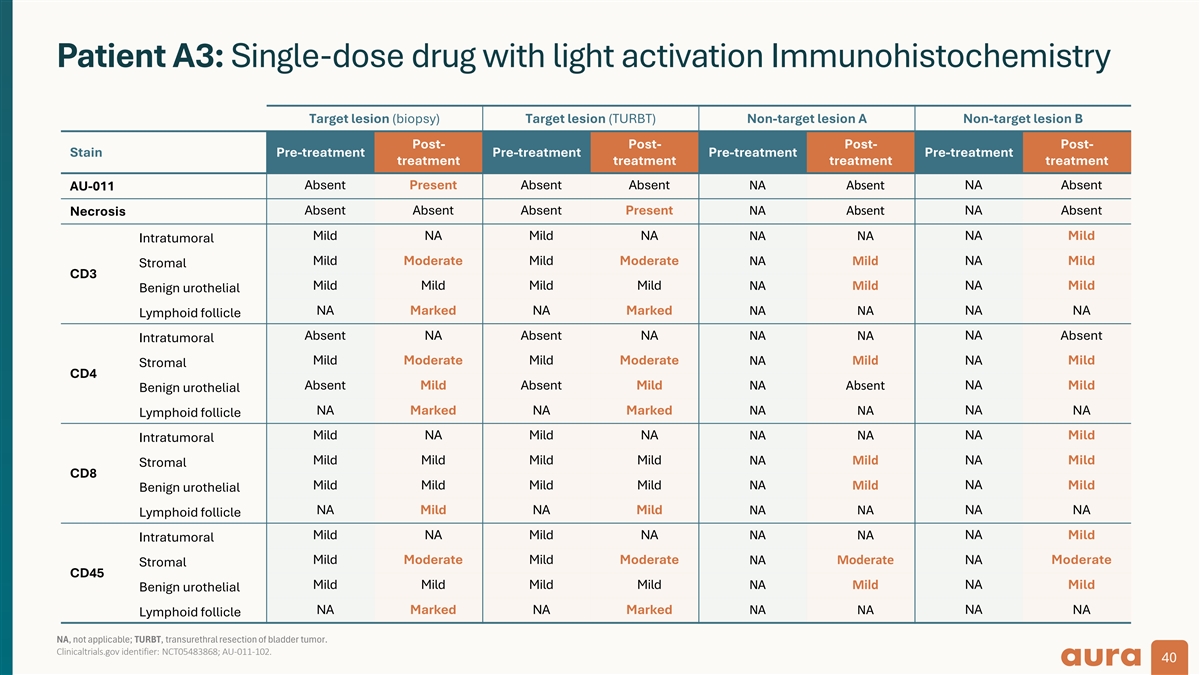
Patient A3: Single-dose drug with light activation Immunohistochemistry Target lesion (biopsy) Target lesion (TURBT) Non-target lesion A Non-target lesion B Post- Post- Post- Post- Stain Pre-treatment Pre-treatment Pre-treatment Pre-treatment treatment treatment treatment treatment Absent Present Absent Absent NA Absent NA Absent AU-011 Absent Absent Absent Present NA Absent NA Absent Necrosis Mild NA Mild NA NA NA NA Mild Intratumoral Mild Moderate Mild Moderate NA Mild NA Mild Stromal CD3 Mild Mild Mild Mild NA Mild NA Mild Benign urothelial NA Marked NA Marked NA NA NA NA Lymphoid follicle Absent NA Absent NA NA NA NA Absent Intratumoral Mild Moderate Mild Moderate NA Mild NA Mild Stromal CD4 Absent Mild Absent Mild NA Absent NA Mild Benign urothelial NA Marked NA Marked NA NA NA NA Lymphoid follicle Mild NA Mild NA NA NA NA Mild Intratumoral Mild Mild Mild Mild NA Mild NA Mild Stromal CD8 Mild Mild Mild Mild NA Mild NA Mild Benign urothelial NA Mild NA Mild NA NA NA NA Lymphoid follicle NA Mild NA Mild NA NA NA Mild Intratumoral Mild Moderate Mild Moderate Moderate Moderate NA NA Stromal CD45 Mild Mild Mild Mild NA Mild NA Mild Benign urothelial NA Marked NA Marked NA NA NA NA Lymphoid follicle NA, not applicable; TURBT, transurethral resection of bladder tumor. Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 40
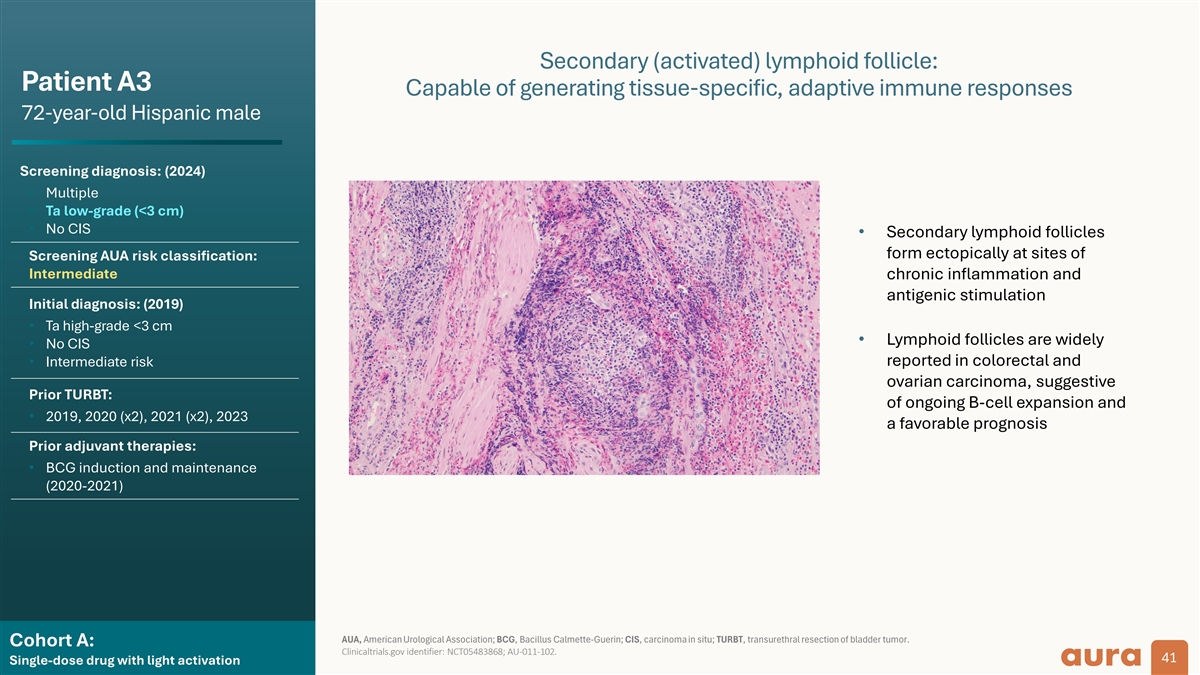
Secondary (activated) lymphoid follicle: Patient A3 Capable of generating tissue-specific, adaptive immune responses 72-year-old Hispanic male Screening diagnosis: (2024) • Multiple • Ta low-grade (<3 cm) • No CIS • Secondary lymphoid follicles form ectopically at sites of Screening AUA risk classification: Intermediate chronic inflammation and antigenic stimulation Initial diagnosis: (2019) • Ta high-grade <3 cm • Lymphoid follicles are widely • No CIS • Intermediate risk reported in colorectal and ovarian carcinoma, suggestive Prior TURBT: of ongoing B-cell expansion and • 2019, 2020 (x2), 2021 (x2), 2023 a favorable prognosis Prior adjuvant therapies: • BCG induction and maintenance (2020-2021) AUA, American Urological Association; BCG, Bacillus Calmette-Guerin; CIS, carcinoma in situ; TURBT, transurethral resection of bladder tumor. Cohort A: Clinicaltrials.gov identifier: NCT05483868; AU-011-102. 41 Single-dose drug with light activation